Rabies is still responsible for approximately 60,000 human deaths per year mostly in Asia and Africa and affects especially underserved people. Yet, since the first vaccine developed by Louis Pasteur more than 130 years ago, prophylactic measures have significantly improved. They are now composed of the vaccine allied to purified human or equine rabies immunoglobulins. However, these immunoglobulins are expensive and not easy to reach in developing settings. Researchers from the Structural Virology Unit at the Institut Pasteur, in collaboration with the Virus and Immunity Unit and the Lyssavirus Epidemiology and Neuropathology Unit, have visualized one of the most potent and most broadly neutralizing human monoclonal antibody in interaction with the rabies glycoprotein. This finding makes it possible to propose new avenues, both prophylactic and therapeutic, in the fight against rabies.
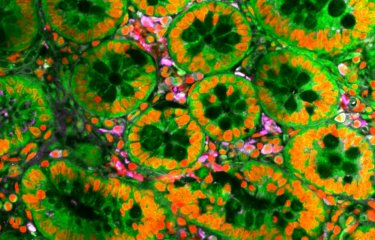
Rabies is a lethal encephalitis due to a lyssavirus mainly transmitted to humans by the bite or scratches of terrestrial carnivores (principally domestic dogs). The onset of clinical symptoms and death can be 100% prevented by adequate post-exposure prophylaxis (PEP) including vaccines and passive immunization using rabies immunoglobulins (read the Institut Pasteur disease sheet). Today, 15 to 29 million of patients exposed to rabies received the PEP each year whose terms have been updated by WHO in 2018 as a result of Institut Pasteur expertise.
“If prevention measures therefore exist today to fight rabies, supply and demand are incoherent in developing countries. The proposed treatments are not produced or not available on site” explains Félix Rey, head of the Structural Virology Unit at the Institut Pasteur.
The RVC20 monoclonal antibody: a key-tool to understand the rabies virus
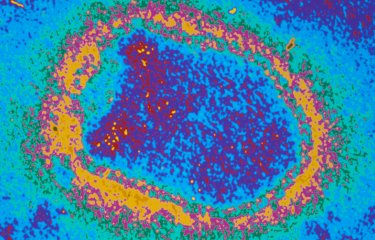
The rabies virus has only one glycoprotein (called G) exposed at its surface. This protein is responsible for the entry of the virus into the human cell and is therefore the only target of neutralising antibodies. In spite of its medical relevance, no structural data are available for the rabies virus surface glycoprotein.
“Here we report the structure of one of the most potent and most broadly neutralizing human monoclonal antibodies (mAb), named RVC20 in complex with the domain of G that it recognizes and binds” explains Hervé Bourhy, head of the Lyssavirus Epidemiology and Neuropathology Unit at the Institut Pasteur.
Researchers have described the crystal structure of the RCV20 antibody in complex with its target domain, one of the major antigenic sites of the rabies virus glycoprotein. The structure reveals that RVC20 involves highly conserved features of the viral glycoprotein, rationalizing its broad reactivity among the virus strains.
“We further show that RVC20 monoclonal antibody blocks the membrane fusion between the virus and the cell” says Hervé Bourhy. The antibody therefore blocks the entry of the virus into the cell and further spreading of the virus within the body of the infected host.
New perspectives for prevention and treatment
“Our study also highlights a major site of vulnerability at the virion surface, providing a mechanistic understanding of highly efficient rabies virus neutralization by the RVC20 antibody” summarizes Félix Rey. The new knowledge provided by this study could be employed not only for mAb-based prophylaxis, but also for future therapeutic applications in cases where the virus has already entered the nervous system and for which there is still no cure. “The idea behind these studies is being able to provide a substitute to the actual post exposure prophylaxis to protect against rabies” concludes Félix Rey.
The results of this study were made possible thanks to the collaboration of two platforms at the Center for Technological Resources and Research at the Institut Pasteur: the Crystallography Platform and the Molecular Biophysics Platform.
Source
Structure of the prefusion-locking broadly neutralizing antibody RVC20 bound to the rabies virus glycoprotein, Nature Communications, January, 30, 2020
Jan Hellert1, Julian Buchrieser2, Florence Larrous3, Andrea Minola4, Guilherme Dias de Melo3, Leah Soriaga5, Patrick England6, Ahmed Haouz7, Amalio Telenti5, Olivier Schwartz2,Davide Corti4, Hervé Bourhy3, Félix A. Rey1
1 Structural Virology Unit, Institut Pasteur, CNRS UMR 3569, 25-28 rue du Docteur Roux, 75724, Paris, Cedex 15, France
2 Virus and Immunity Unit, Institut Pasteur, CNRS UMR 3569, 25-28 rue du Docteur Roux, 75724, Paris, Cedex 15, France
3 Lyssavirus Epidemiology and Neuropathology Unit, Institut Pasteur, 25-28 rue du Docteur Roux, 75724, Paris, Cedex 15, France
4 Humabs BioMed SA, a subsidiary of Vir Biotechnology Inc., Via dei Gaggini 3, 6500, Bellinzona, Switzerland
5 Vir Biotechnology Inc., San Francisco, CA 9415822
6 Molecular Biophysics Platform C2RT, Institut Pasteur, CNRS UMR 3528, 25-28 rue du Docteur Roux, 75724, Paris, Cedex 15, France
7 Crystallography Platform C2RT, Institut Pasteur, CNRS UMR 3528, 25-28 rue du Dr. Roux, 75724, Paris, Cedex 15, France