The malaria molecular epidemiology unit at the Institut Pasteur in Cambodia is interested in the resistance of the malaria pathogens to the drugs currently in use, in particular to the molecular markers making to identify this resistance. Researchers working in this unit have contributed to the identification of a marker associated with resistance to artemisinin in 2014 and one associated with resistance to piperaquine in 2016. Benoit Witkowski, researcher in this unit, discusses the challenges of antimalarial resistance.
In the late 1960s, resistance to the first generation of malaria drugs emerged in Southeast Asia. Is the danger still coming from this part of the world today?
The first cases of problematic resistance to mainstream antimalarial, such as chloroquine (Nivaquine), appeared at the border between Cambodia and Thailand. Subsequently, these resistances through parasites migrated to sub-Saharan Africa, greatly increasing mortality in the 1980s and 1990s. We do not want history to repeat itself! New drugs have been introduced, Artemisinin-based Combination Therapy (ACT), which are a combination of drugs between an active ingredient called artemisinin and older antimalarials. These are the basic treatment of malaria at the present time. The problem is that in Cambodia, we have observed in the parasites the development of resistance to both artemisinin and, more worryingly, to partner compounds. They are now multi-resistant parasites.
Against these multiresistant parasites, drugs are not enough or no longer effective?
The last used, dihydroartemisinin-piperaquine, showed treatment failure rates of about 60%, ie 60% of patients treated were not cured of malaria. For the moment, this resistance is characterized by late treatment failures - the symptoms reappear one month after the treatment. There is an effect on the parasite but it is not enough to eliminate it, which means that these medicines, we counted on to limit the prevalence of malaria, will no longer be effective enough.
Therefore, the challenge is twofold: to find therapeutic solutions to fight against these parasites and to monitor the potential migration of these resistant parasites to Africa, which would be catastrophic from the health point of view because of the much higher transmission rate.
How can the emergence of these resistances be followed?
The detection of resistances is primarily clinical, ie the first step is to identify if a treatment no longer works optimally. Once this problem is determined, it is important to have tools to quickly define the proportion of resistant parasites in a given area. One of our activities is to set up the molecular monitoring tools, ie we will determine by DNA analysis of the parasite which genetic modifications generate resistance, it can be a mutation in a gene or a gene that duplicates in the genome.
This is what we call a molecular resistance marker and once this tool is obtained, it is then possible to monitor the presence or absence of resistant parasites on thousands of samples.
What to do when you spot resistances?
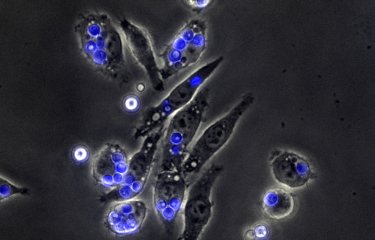
It is still possible to "juggle" with the various ACTs: for example, in Cambodia DHA-piperaquine has been replaced by a combination of artesunate with mefloquine, which seems to be so far very active. But this may not last. This solution remains an emergency solution and the common pharmacological basis of ACTs will force us to turn to new compounds. This is also one of our activities for which we evaluate in vitro new antimalarials capable of acting against the multiresistant parasites of Cambodia.
Are there many new molecules in the pipeline, knowing that malaria is not a priority for pharmaceutical companies?
There are many, but the development of a new drug takes a long time. It is difficult to know how many will finally come to the market one day. Nevertheless, several pahrma company are currently investing and clinical trials of new drugs will be conducted soon in Asia.