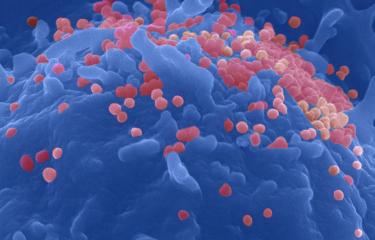
Some rare HIV-infected patients are able to keep the viral load low enough not to require treatment. A study by researchers at the Pasteur Institute and collaborators shows that these patient CD4+ T cells block a receptor that is important for HIV entry.
HIV controllers are rare patients who naturally control HIV replication in the absence of antiretroviral therapy. These patients are known to harbor particularly efficient antiviral T cells, that help maintain the population of infected cells to very low levels. HIV preferentially targets and destroys activated CD4+ T cells, known as “helper cells”. Antiviral CD4+ T cells themselves become activated upon encounter with the virus. How these cells escape depletion in controllers, however, remains incompletely understood. A recent study by Institut Pasteur and Inserm researchers shows that antiviral CD4+ T cells of controllers express lower levels of the coreceptor CCR5, resulting in a lower susceptibility to HIV entry. These findings are published in Nature Communications.
Lower expression of a chemokine receptor
HIV controllers, who represent fewer than 0.5% of infected individuals, can remain healthy for decades without receiving antiviral treatment. The French agency for AIDS Research, ANRS-MIE, has implemented the HIV controller CODEX cohort at the national level, to enable studies of the mechanisms involved in AIDS resistance. It was already known that HIV controllers were endowed with potent antiviral cytotoxic CD8+ T cells capable of efficiently killing infected cells. Previous CODEX studies had also shown that controllers CD4+ T cells were highly sensitive to viral antigens, and could thus keep the immune system in constant alert, by rapidly activating and providing help to other immune effectors as soon as the virus started to replicate. However, it remained unclear how these antiviral CD4+ T cells, which were the first to activate upon HIV encounter, could avoid being immediately infected and destroyed by the very same virus.
Research conducted by the group of Lisa Chakrabarti, in the Virus and Immunity Unit at the Institut Pasteur, in collaboration with the clinical team of Olivier Lambotte at Inserm, provides an explanation of the persistence of a population of antiviral CD4+ T cells in HIV controllers. With the support of the UTechS platform Cytometry and Biomarkers, the researchers found that CD4+ T cells capable of recognizing HIV antigens express lower levels of a chemokine receptor, named CCR5, in HIV controllers than in treated patients. As CCR5 plays a key role as a coreceptor for HIV entry, lower CCR5 expression makes these specific CD4+ T cells less susceptible to HIV infection.
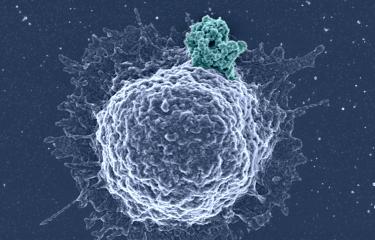
Blocking the virus gateway
Two mechanisms were involved in the lower CCR5 expression observed in HIV controllers. In rare cases, controllers carried a combination of genetic mutations that impaired CCR5 expression at the cell surface. However, in the majority of them, CCR5 was functionally down-regulated by an abundant production of its ligands, the beta-chemokines. Indeed, the antiviral CD4+ T cells of controllers were strongly activated through their T cell receptor upon HIV antigen encounter, resulting in intracellular signals that induced a persistent secretion of beta-chemokines. These chemokines in turn bound CCR5 at the surface of activated CD4+ T cells, resulting in an internalization of the receptor.
These findings show that CCR5 down-regulation plays a key role in natural HIV control, and suggest that strategies that aim at inactivating or blocking CCR5 may contribute to the development of HIV cure strategies.
This work was supported by a grant from PasteurInnov TETRHIS.
This study is part of the priority scientific area Emerging infectious diseases of the Institut Pasteur's strategic plan for 2019-2023.
Source:
Low CCR5 expression protects HIV-specific CD4+ T cells of elite controllers from viral entry, Nature Communications, January 26, 2022
Mathieu Claireaux1,2, Rémy Robinot1,2, Jérôme Kervevan1,2, Mandar Patgaonkar1,2,
Isabelle Staropoli1,2, Anne Brelot1,2, Alexandre Nouël1,2, Stacy Gellenoncourt1,2, Xian Tang1,2, Mélanie Héry1,2, Stevenn Volant3, Emeline Perthame3, Véronique Avettand-Fenoël4,5, Julian Buchrieser1,2, Thomas Cokelaer3,6, Christiane Bouchier6, Laurence Ma6, Faroudy Boufassa7, Samia Hendou7, Valentina Libri8, Milena Hasan8, David Zucman9, Pierre de Truchis10, Olivier Schwartz1,2, Olivier Lambotte11,12, Lisa A. Chakrabarti1,2
1 - Unité Virus et immunité, Institut Pasteur, Université de Paris, Paris, France.
2 - CNRS UMR3569, Paris, France.
3 - Hub de Bioinformatique et biostatistique, département Biologie computationnelle, Institut Pasteur, Université de Paris, Paris, France.
4 - AP-HP Hôpital Necker-Enfants malades, Laboratoire de microbiologie clinique, Paris, France.
5 - CNRS 8104, INSERM U1016, Université Paris-Descartes, Sorbonne Paris Cité, Faculté de médecine, Paris, France.
6 - Plateforme Biomics, C2RT, Institut Pasteur, Université de Paris, Paris, France.
7 - INSERM U1018, Centre de recherche en épidémiologie et santé des populations (CESP), Le Kremlin-Bicêtre, France.
8 - Cytométrie et biomarqueurs (UTechS CB), Centre de recherche translationnelle, Institut Pasteur, Université de Paris, Paris, France.
9 - Unité VIH, Hôpital Foch, Suresnes, France.
10 - AP-HP, service des maladies infectieuses et tropicales, Hôpital Raymond Poincaré, Garches, France.
11 - INSERM U1184, Université Paris-Sud, CEA, service Immunologie des infections virales et des maladies auto-immunes, Le Kremlin-Bicêtre, France.
12 - AP-HP, service Médecine Interne et immunologie clinique, Hôpitaux universitaires Paris-Sud, Le Kremlin-Bicêtre, France.