Our microbiota provide an additional means of fighting off infections but can be adversely affected by antibiotic therapy. A study modeling microbial populations and their response to drugs offers potential for improving our understanding of antibiotic resistance and tackling it more effectively.
Antibiotic resistance is a major public health issue and an increasingly serious threat. Besides developing effective new drugs to fight single and multidrug-resistant bacteria, research also focuses on developing other care and prevention techniques aimed at circumventing resistance phenomena. Epidemiologists David Smith, Laura Temime and Lulla Opatowski at the Institut Pasteur have examined the potential role of our microbiota in the spread of resistant bacteria.
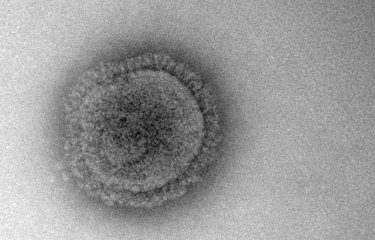
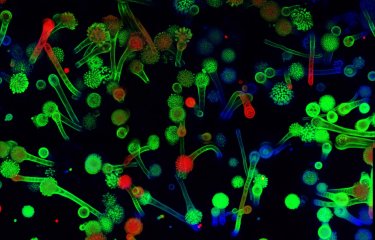
As a reminder, the term "microbiota" refers to all microorganisms that live in and on our body and interact with it. Although we only partially understand the roles they play in relation to our health, it is very likely that infectious bacteria are in competition with other microbiota bacteria. When antibiotics are administered, the "good" bacteria susceptible to drugs are eliminated, giving free rein to pathogens if these are more resistant. This therefore provides conditions conducive to their multiplication and spread as they have easier access to resources.
This is the process described in the study, which used mathematical modeling to gain insights into changes in bacterial populations when faced with antimicrobial agents. "Our models have enabled us to examine competition between these resistant bacteria and microbiota present in the body", explains David Smith from the Epidemiology and Modelling of Antibiotic Evasion Unit. By analyzing the impact of antibiotic consumption on these microbiota and extrapolating to the risk of outbreaks at population level, the scientists were able to assess the positive role of antibiotics in terms of their ability to eliminate bacterial infections, as well as their negative role, which is dependent on the antibiotic susceptibility of microbiota as a whole. As well as potentially keeping people healthy, microbiota could therefore also provide a means of tackling drug-resistant bacteria.
Given this finding, the scientists are now assessing strategies for combating antimicrobial resistance in hospitals. Clearly there is a need to limit the mass use of antibiotics. However, it is also important to use them more effectively and help microbiota recover after use through appropriate treatments. These combined measures offer a potential means of limiting the spread of increasingly resistant bacterial strains that are gradually being selected due to antibiotic use and are developing mutations capable of preventing drugs from taking effect.
This study is part of the priority scientific area Antimicrobial Resistance of the Institut Pasteur's strategic plan for 2019-2023.
Microbiome-pathogen interactions drive epidemiological dynamics of antibiotic resistance: a modelling study applied to nosocomial pathogen control, eLife, 14 septembre 2021
David R. M. Smith1,2,3, Laura Temime3,4, Lulla Opatowski1,2
1. Institut Pasteur, Epidemiology and Modelling of Antibiotic Evasion (EMEA), Paris, France
2. Université Paris-Saclay, UVSQ, Inserm, CESP, Anti-infective evasion and pharmacoepidemiology team, Montigny-Le-Bretonneux, France
3. Modélisation, épidémiologie et surveillance des risques sanitaires (MESuRS), Conservatoire national des arts et métiers, Paris, France
4. PACRI unit, Institut Pasteur, Conservatoire national des arts et métiers, Paris, France