By June 2022, the Wallis and Futuna Islands, a French overseas territory, had successfully implemented a Zero-COVID strategy that significantly reduced the number of SARS-CoV-2 infections. From mid-June 2022, a gradual reopening of the borders was planned. However, the relatively low immunity in the population (due to limited vaccination coverage and the number of previous infections) and the high prevalence of comorbidities (70% of adults are obese and 15% diabetic) led to fears of a resurgence of the epidemic with a significant impact on health. In this context, and with a view to advising the health authorities, scientists from the Institut Pasteur, the CNRS and Université Paris Cité developed mathematical models to predict how this wave of the epidemic could be mitigated through increased vaccination and the use of the antiviral Paxlovid®. The results, which attest to the valuable role of modelling in managing the COVID-19 epidemic, were published in The Lancet Regional Health – Western Pacific on November 14, 2022.
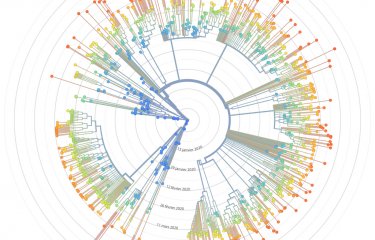
As part of this study, which was conducted in collaboration with the Wallis and Futuna health agency, scientists from the Mathematical Modelling of Infectious Diseases Unit (Institut Pasteur/CNRS Evolutionary Genomics, Modelling and Health Unit/Université Paris Cité), led by Simon Cauchemez, considered two types of pharmaceutical measures: the use of Paxlovid® (nirmatrelvir/ritonavir), an antiviral drug that has been shown to reduce the risk of hospitalisation in people at risk of severe forms of the disease, and increased vaccination coverage. The geographic features of Wallis and Futuna meant that the level of virus transmission in the region was uncertain. The modelers therefore considered three levels of SARS-CoV-2 transmission intensity: low (R0=3), medium (R0=5) (a scenario in which the epidemic growth corresponded to that observed in mainland France during the first Omicron wave in December 2021), and high (R0=7). The baseline reproduction number, R0, here describes the average number of people infected by a single case, in a scenario in which there is no population immunity, but in which non-pharmaceutical control measures, such as mask-wearing, could reduce transmission. Finally, the population was divided into three groups according to the type of comorbidities that increase the risk of hospitalisation.
The scientists estimated that the epidemic would begin between 13 and 20 days after the borders were reopened. In the absence of any pharmaceutical measures, the number of patients requiring hospitalisation was estimated to be between 115 and 156 in the medium-transmissibility scenario (R0=5) and between 68 and 100 in the low-transmissibility scenario (R0=3). Treatment with Paxlovid® of 50% of patients over 65 years of age with comorbidities and of those over 40 years of age with significant comorbidities could reduce the number of hospitalisations by 11% to 21%, depending on the effectiveness of the treatment (50% to 90%). This scenario would require between 403 and 481 patients to be treated. Improved vaccination coverage through booster doses could reduce hospitalisations by 15%. The burden of hospitalisation would be reduced even further by combining the use of Paxlovid® with increased vaccination coverage. The model also showed that expanding the target population for treatment with Paxlovid® could further reduce the number of people requiring hospitalisation.
As expected, after reopening the borders, a COVID-19 outbreak occurred in the islands in July and August 2022, which enabled the scientists to compare their projections with the observed data. The onset of the epidemic occurred 17 days after the end of the Zero-COVID strategy, consistent with model projections (13-20 days). The dynamics of the epidemic were similar to those anticipated in the most optimistic scenario of low transmission intensity (R0=3). The model aligned well with the observed dynamics of cases, hospital admissions and the number of patients treated with Paxlovid®. However, the model overestimated the number of beds required at the peak of the epidemic, because the length of hospitalisation observed in Wallis and Futuna was shorter (4 days) than that of the model (11 days), which was based on data from mainland France.
"This model has been useful in helping authorities plan for the end of Zero-COVID in Wallis and Futuna. It also quantified how the use of Paxlovid® could lessen the impact of the expected epidemic wave after exiting the Zero-COVID strategy in a setting with a high prevalence of comorbidities", says Simon Cauchemez, Head of the Institut Pasteur's Mathematical Modelling of Infectious Diseases Unit.
Source
Modelling the end of a Zero-COVID strategy using nirmatrelvir/ritonavir, vaccination and NPIs in Wallis and Futuna, The Lancet Regional Health – Western Pacific, November 14, 2022
Antoine Braulta, Cécile Tran-Kiema,b, Clément Couteauxc, Valérie Oliéd, Juliette Paireaua,d, Yazdan Yazdanpanahe, JadeGhosne, Guillaume Martin-Blondelf, Paolo Bosettia,g, Simon Cauchemeza,g,*
a Mathematical Modelling of Infectious Diseases Unit, Institut Pasteur, Université Paris Cité, CNRS UMR 2000, Paris, France
b Collège doctoral, Sorbonne Université, Paris, France
c Agence de Santé de Wallis-et-Futuna, France
d Santé publique France, France
e Infections Antimicrobials Modelling Evolution (IAME), INSERM UMR 1137, Université Paris Cité, Paris, France
f Service des Maladies Infectieuses et Tropicales, CHU de Toulouse, Institut Toulousain des Maladies Infectieuses et Inflammatoires (Infinity), INSERM UMR 1291 - CNRS UMR 5051 - Université Toulouse III, France
g Equal senior contribution
*Corresponding author