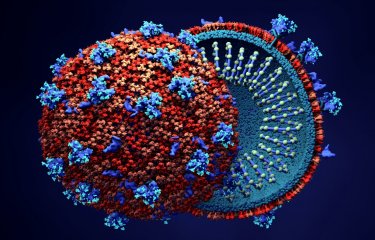
People living with HIV need to take antiretroviral treatment for life to prevent the virus from multiplying in their body. But some people, known as "post-treatment controllers," have been able to discontinue their treatment while maintaining an undetectable viral load for several years. Starting treatment early could promote long-term control of the virus if treatment is discontinued. Scientists from the Institut Pasteur, the CEA, Inserm, Université Paris Cité and Université Paris-Saclay, in collaboration with Institut Cochin1 and with the support of MSD Avenir and ANRS Emerging Infectious Diseases, used an animal model to identify a window of opportunity for the introduction of treatment that promotes remission of HIV infection: it appears that starting treatment four weeks after infection promotes long-term control of the virus following the interruption of treatment after two years of antiretroviral therapy. These results highlight how important it is for people with HIV to be diagnosed and begin treatment as early as possible. The findings were published in the journal Nature Communications on January 11, 2024.
Research on the VISCONTI cohort, composed of 30 post-treatment controllers, has provided proof of concept of possible long-term remission for people living with HIV. These individuals received early treatment that was maintained for several years. When they subsequently interrupted their antiretroviral treatment, they were capable of controlling viremia for a period lasting more than 20 years in some cases. At the time (in 2013), the team leading the VISCONTI study suggested that starting treatment early could promote control of the virus, but this remained to be proven.
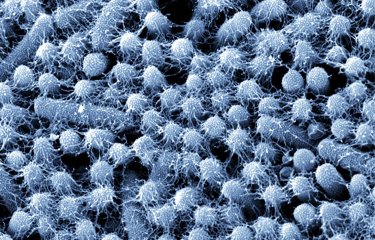
In this new study, the scientists used a primate model of SIV2 infection which allowed them to control all the parameters (sex, age, genetics, viral strain, etc.) that may have an impact on the development of immune responses and progression to disease. They compared groups that had received two years of treatment, starting either shortly after infection (in the acute phase) or several months after infection (in the chronic phase), or no treatment.
The reproducible results show that starting treatment within four weeks of infection (as was the case for most of the participants in the VISCONTI study) strongly promotes viral control after discontinuation of treatment. This protective effect is lost if treatment is started just five months later. "We show the link between early treatment and control of infection after treatment interruption, and our study indicates that there is a window of opportunity to promote remission of HIV infection," comments Asier Sáez-Cirión, Head of the Institut Pasteur's Viral Reservoirs and Immune Control Unit and co-last author of the study.
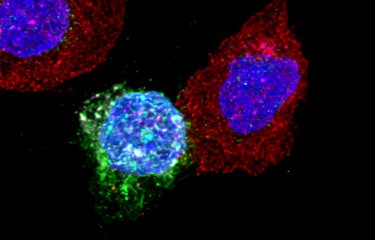
The scientists also demonstrated that early treatment promotes the development of an effective immune response against the virus. Although the antiviral CD8+ T immune cells developed in the first weeks after infection have very limited antiviral potential, the early introduction of long-term treatment promotes the development of memory CD8+ T cells, which have a stronger antiviral potential and are therefore capable of effectively controlling the viral rebound that occurs after treatment interruption. "We observed that early treatment maintained for two years optimizes the development of immune cells. They acquire an effective memory against the virus and can eliminate it naturally when viral rebound occurs after discontinuation of treatment," explains Asier Sáez-Cirión.
These results confirm how important it is for people with HIV to be diagnosed and begin treatment as early as possible. "Starting treatment six months after infection, a delay that our study shows results in a loss of effectiveness, is already considered as a very short time frame compared with current clinical practice, with many people with HIV starting treatment years after infection because they are diagnosed too late," notes Roger Le Grand, Director of IDMIT (Infectious Disease Models for Innovative Therapies) and co-last author of the study. "Early treatment has a twofold effect: individually, as early treatment prevents diversification of the virus in the body and preserves and optimizes immune responses against the virus; and collectively, as it prevents the possibility of the virus spreading to other people," adds Asier Sáez-Cirión.
Finally, these results should guide the development of novel immunotherapies targeting the immune cells involved in the remission of HIV infection.
These are the initial results of the p-VISCONTI study, which began in 2015 in collaboration with the institutions cited above and received funding from MSD Avenir and the support of ANRS Emerging Infectious Diseases as part of the RHIVIERA consortium.
1 Institut Cochin is a biomedical research center affiliated with Inserm, the CNRS and Université Paris Cité.
2 SIV: simian immunodeficiency virus only affects non-human primates. SIV infection of animals recapitulates the key features of human HIV infection.
Source
Early antiretroviral therapy favors post-treatment SIV control associated with the expansion of enhanced memory CD8+ T-cells, Nature Communications, January 11, 2024
Caroline Passaes1,2*, Delphine Desjardins3, Anaïs Chapel1,2, Valérie Monceaux1,2, Julien Lemaitre3, Adeline Melard4, Federico Perdomo-Celis2, Cyril Planchais5, Maël Gourvès1, Nastasia Dimant3, Annie David2, Nathalie Dereuddre-Bosquet3, Aurélie Barrail-Tran3,6, Hélène Gouget3, Céline Guillaume3, Francis Relouzat3, Olivier Lambotte3,7, Jeremie Guedj8, Michaela Müller-Trutwin2, Hugo Mouquet5, Christine Rouzioux9, Veronique Avettand-Fenoel4,10, Roger Le Grand3,#, Asier Sáez-Cirión1,2,#
1 Institut Pasteur, Université Paris Cité, Viral Reservoirs and Immune Control Unit Paris, France.
2 Institut Pasteur, Université Paris Cité, HIV Inflammation and Persistence Unit, Paris, France.
3 Université Paris-Saclay, CEA, Inserm, UMR1184, Immunology of Viral, Auto-immune, Hematological and Bacterial diseases (IMVA-HB/IDMIT Department), Fontenay-aux-Roses/Le Kremlin-Bicêtre, France.
4 Université Paris Cité; Inserm, U1016 ; CNRS, UMR8104, Paris, France.
5 Institut Pasteur, Université Paris Cité, Inserm U1222, Humoral Immunology Unit, Paris, France.
6 Université Paris-Saclay, AP-HP, Hôpital Bicêtre, Service de Pharmacie, Le Kremlin Bicêtre, France.
7 Université Paris-Saclay, AP-HP. Hôpital Bicêtre, Clinical Immunology Department, 94270, Le Kremlin Bicêtre, France.
8 Université Paris Cité, IAME, Inserm, F-75018 Paris, France.
9 Université Paris Cité/APHP Hôpital Necker - Enfants Malades, Paris France.
10 APHP Hôpital Cochin, Service de Virologie, Paris France.
# equal contribution