Disease outbreaks are unpredictable and often deadly. Wherever they occur on the planet, we are all potentially at risk: in our era of globalized air travel, a microbe can make it round the world in less than 24 hours. Alongside outbreaks of well-established diseases such as influenza, yellow fever, plague, cholera and measles, we are also seeing many outbreaks caused by more "recent" pathogens identified since the 1970s, including HIV, SARS, hepatitis C, MERS-CoV and Ebola. And other emerging viruses, such as Nipah virus in Asia and monkeypox in Africa, are now beginning to raise concerns among scientists.
The profile of a pandemic virus
What might a pathogen at high risk of rapidly causing a dangerous pandemic (a disease outbreak affecting more than one continent) look like? If we were to piece together an identikit picture, it would have the following characteristics: a virus that is easily spread between humans through airborne transmission, is highly contagious before the emergence of the first symptoms, has a short incubation period and is fatal in more than one in a thousand cases. Bearing this in mind, the influenza virus remains one of the most feared, and highly monitored, diseases (see inset). The reassortment of influenza virus genomes in humans, birds and pigs is constantly creating new viruses with the potential to be more pathogenic than those responsible for seasonal flu outbreaks – which themselves cause high numbers of deaths (9,900 last winter in France). An influenza virus to which no one is immune could affect between 20 and 50% of the world's population. As Dr. Tedros Adhanom Ghebreyesus, Director-General of the World Health Organization (WHO), said recently, "The ongoing risk of a new influenza virus transmitting from animals to humans and potentially causing a pandemic is real. The question is not if we will have another pandemic, but when."
The biggest pandemic in recent decades, however, has been caused by HIV. Its very slow incubation period – 10 years on average before the emergence of the first symptoms, although the infected individual is already contagious – explains why it has affected so many people: 35 million deaths and 37 million people currently infected.

The Institut Pasteur on the front line to tackle disease outbreaks in France and worldwide
Influenza, meningitis, salmonella, etc.: in France, the Institut Pasteur is in charge of monitoring several pathogens via its 14 "National Reference Centers" (CNRs), designated by the French General Directorate of Health (DGS). CNRs serve as infectious disease observatories and raise the alert in the event of an outbreak. The Institut Pasteur's Laboratory for Urgent Response to Biological Threats (CIBU), on constant standby 24/7, also plays a major part in these efforts. The CIBU was particularly active during the 2009 H1N1 influenza pandemic, supporting the CNR for Influenza in diagnosing French cases. "We also carry out regular missions abroad, like in 2015 in Guinea, where we organized screening for the Ebola virus during the outbreak," explains CIBU head Jean-Claude Manuguerra.
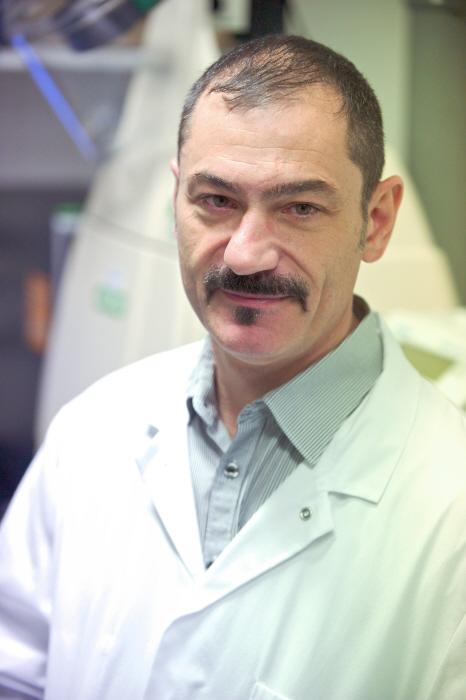
We also carry out regular missions abroad, like in 2015 in Guinea, where we organized screening for the Ebola virus during the outbreak.
Jean-Claude ManuguerraHead of the Institut Pasteur's Laboratory for Urgent Response to Biological Threats
These missions are now carried out in collaboration with the Outbreak Investigation Task Force (OITF), composed of volunteers in various disciplines (microbiologists, epidemiologists, entomologists, etc.) from the Institut Pasteur in Paris and the Institut Pasteur International Network. These specialists in infection prevention and control are ready to be deployed anywhere in the world. They respond to WHO calls for assistance issued via its Global Outbreak Alert and Response Network (GOARN), of which the Institut Pasteur is a member. In 2018, experts were sent to tackle a listeriosis outbreak in South Africa, to a camp of Rohingya refugees suffering from diphtheria in Bangladesh, and to deal with the Ebola outbreak in the Democratic Republic of the Congo and in neighboring countries at risk (Rwanda and Burundi). Specialists can also be sent directly by the Institut Pasteur in Paris, as was the case during the pneumonic plague outbreak in Madagascar in 2017: as hundreds of cases were reported, 11 Institut Pasteur scientists were deployed to the field to help the Institut Pasteur de Madagascar and local health authorities bring the situation under control.
*Outbreak investigation task force.

From air travel to climate change
Regardless of the pathogen involved, several factors encourage the occurrence of disease outbreaks. These include a growing world population which quadrupled over the 20th century, together with the concentration of populations in megacities; air travel, which for example enabled severe acute respiratory syndrome (SARS) to reach six countries, including Canada, in less than a week after it first emerged in China in 2002; conflict (a cholera outbreak recently hit Yemen); deforestation, which is bringing humans into contact with animals that are vectors of new pathogens (60% of emerging viruses in humans come from animals); and climate change, which is responsible for the spread of the tiger mosquito – a potential vector of chikungunya, dengue and Zika (see Interview) – to France, where it can now be found in 66 mainland departments, and to Europe, representing a new threat.
Vector control (mosquito eradication, rat extermination, etc.) and monitoring animals with the potential to transmit pathogens (birds, rodents, bats, etc.) are two key weapons in the outbreak prevention arsenal. What other strategies are there?
Understanding human behavior
With her "Medical anthropology and environment" group at the Institut Pasteur, Tamara Giles-Vernick conducts field studies on various health issues among local populations. One of her studies, carried out in south-eastern Cameroon, looked at the interactions between local residents and monkeys, which are often reservoirs of pathogens that are dangerous for humans (HIV, which originated in monkeys, emerged in this world region). Their hunting and consumption habits represent a potential risk of contamination. "We base our research on open dialog with local residents. We have to develop a relationship of trust with them if we are to understand their daily lives, especially when it comes to sometimes illegal practices such as hunting," explains the anthropologist. "By monitoring villagers over a period of several months, we were able to determine and quantify their contacts with nine species of monkey. We observed that they had more frequent contacts with smaller species than larger monkeys (gorillas and chimpanzees). "

We base our research on open dialog with local residents. We have to develop a relationship of trust with them if we are to understand their daily lives, especially when it comes to sometimes illegal practices such as hunting.
Tamara Giles-VernickHead of the "Medical anthropology and environment" group at the Institut Pasteur
Examining behavior can help improve efforts to combat disease: we demonstrated, for example, that hunters are not the only individuals that need to be targeted. It is important to promote safe methods for handling bushmeat." Tamara coordinates the European Sonar-Global project, a network of social science centers set up to tackle infectious diseases. "As part of this project, we are going to launch a study in Uganda – in a district near the Democratic Republic of the Congo, where there is currently an Ebola outbreak – to assess the population's vulnerability to the virus, which represents a threat to the entire region. Widows and single women could be most at risk."
Research of this type can give rise to recommendations that are useful for health authorities and NGOs.

Know your enemy
The first step is the rapid identification of the infectious agent responsible for the outbreak. Nowadays scientists do not even need to know what they are looking for: high-throughput sequencing can determine the genome of an unknown pathogen in two to four weeks, compared with the two years it took to isolate HIV in the 1980s and the two months needed in 2003 for the SARS virus. Once the pathogen has been characterized, a diagnostic test can be developed.
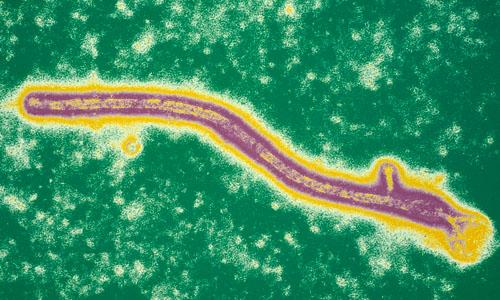
This enables a more rapid response to the crisis – scientists are able to identify the first areas affected by an outbreak and immediately introduce measures to eradicate it. Unfortunately, poor health infrastructures in many countries can hinder this response. When Ebola struck West Africa, four months were lost after the first case before a sample was sent to the National Reference Center for Hemorrhagic Fevers in Lyon, which made the diagnosis. The outbreak claimed 11,300 lives in Guinea, Sierra Leone and Liberia between late 2013 and March 2016.
Improving surveillance
It is therefore vital to improve infectious disease surveillance worldwide. WHO's Global Outbreak Alert and Response Network (GOARN) and its 200 member institutes carry out monitoring and, in the event of an outbreak, send teams to the field to take samples for diagnosis, provide initial treatment and organize any quarantine or vaccination measures (see inset). Preparedness plans are drawn up, including simulation exercises. Under the International Health Regulations, states are obliged to notify any outbreaks that occur within their borders, but the potential impact on the economy and tourism means that some countries are reluctant to cooperate, or only do so too late.

Prediction and anticipation using modeling approaches
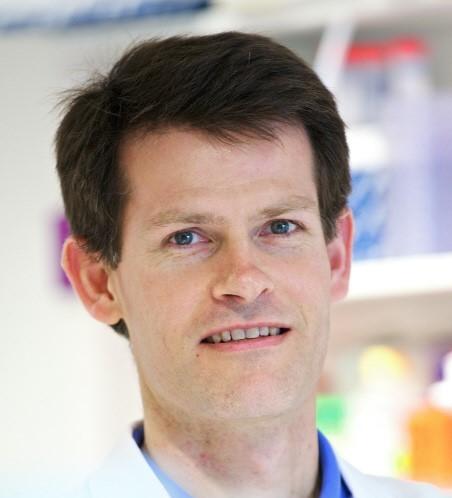
The Mathematical Modeling of Infectious Diseases Unit at the Institut Pasteur uses modeling to predict how outbreaks will develop and analyze the outbreak risk of emerging viruses. "We work closely with Santé publique France to try to answer very specific questions and help the health authorities with their decision-making in the event of a crisis," explains unit head Simon Cauchemez. "During the Zika outbreak in Martinique in 2016, for example, the challenge was to predict how many people would develop neurological complications such as Guillain-Barré syndrome (GBS). Although these cases were rare, the patients required ventilation in intensive care units. Since there were only eight ventilators on the island, the authorities wanted to know whether this would be enough. Using mathematical modeling, and basing our work on a previous outbreak in French Polynesia, we determined various possible scenarios. After a period of uncertainty, the arrival of new data on the outbreak demonstrated that transmissibility was lower than in French Polynesia, and our predictions on the number of GBS cases proved to be relatively accurate."

We have identified which patients particularly need to be placed in isolation. This could help control the propagation of the virus if an outbreak were to occur.
Simon CauchemezHead of the Mathematical Modeling of Infectious Diseases Unit at the Institut Pasteur
The work of the Institut Pasteur team also involves preparing for potential future outbreaks. It recently contributed to a study* on Nipah virus. This virus, transmitted by bats and found throughout South and South East Asia, is fatal in 70% of cases, and there is no treatment or vaccine. WHO believes that it could evolve to become more transmissible, triggering severe outbreaks in the near future. An analysis of epidemiological data over the past 14 years in Bangladesh, the country most affected, showed that adults with respiratory symptoms were more contagious and that contacts of these patients (such as spouses), especially those exposed to respiratory secretions, had a higher likelihood of infection. "We have identified which patients particularly need to be placed in isolation. This could help control the propagation of the virus if an outbreak were to occur," concludes Simon Cauchemez.
Predicting the development of an outbreak
Although we are unable to predict whether an outbreak will occur, we can predict how it might develop by using mathematical modeling techniques. This approach does not tell us exactly how an outbreak will behave, but it does allow us to anticipate several possible scenarios, which are refined as new epidemiological data is collected, and this can help health authorities in their decision-making (see inset).
Social sciences also play an important part in improving our response to health crises. Field surveys carried out by anthropologists (see inset) analyze practices that can encourage the spread of pathogens, for example – as traditional funeral rites did for Ebola –, or rumors that hinder control methods.
Finally, vaccine research is crucial if we are to have a chance of preventing outbreaks. It is worth remembering that the smallpox virus was eradicated from the planet as a result of vaccination, and polio is now only found in a handful of world regions. Vaccine candidates for dengue, Ebola and Zika are currently under study.
Measles is making a comeback
But having an effective vaccine is not enough – as the case of measles shows. This airborne infection, which can cause serious complications, was responsible for up to 2.5 million deaths every year before the introduction of vaccination in 1963. The vaccine was safe and inexpensive, and it prevented millions of deaths. But the infection is coming back, and outbreaks are occurring in several countries. The number of cases worldwide doubled between 2017 and 2018, and 3,000 cases were diagnosed in France last year. Because of the highly contagious nature of the virus (an individual can contaminate between 15 and 20 people), a 95% vaccine coverage rate is needed to stop the disease from spreading. In France, the current figure is barely above 80%. In February 2019, a French family traveling to Costa Rica reintroduced the measles virus to a country that had had no cases since 2014. The reported case of measles in the five-year-old child, who had not been vaccinated and caught the disease before traveling to Costa Rica, led to the family being quarantined and to emergency vaccinations being given to around a hundred people who had come into contact with them. "Being protected also means protecting others": this episode once again shows that vaccination, a powerful weapon in preventing disease outbreaks, is not just a question of individual interest – it is also vital for the collective interest.
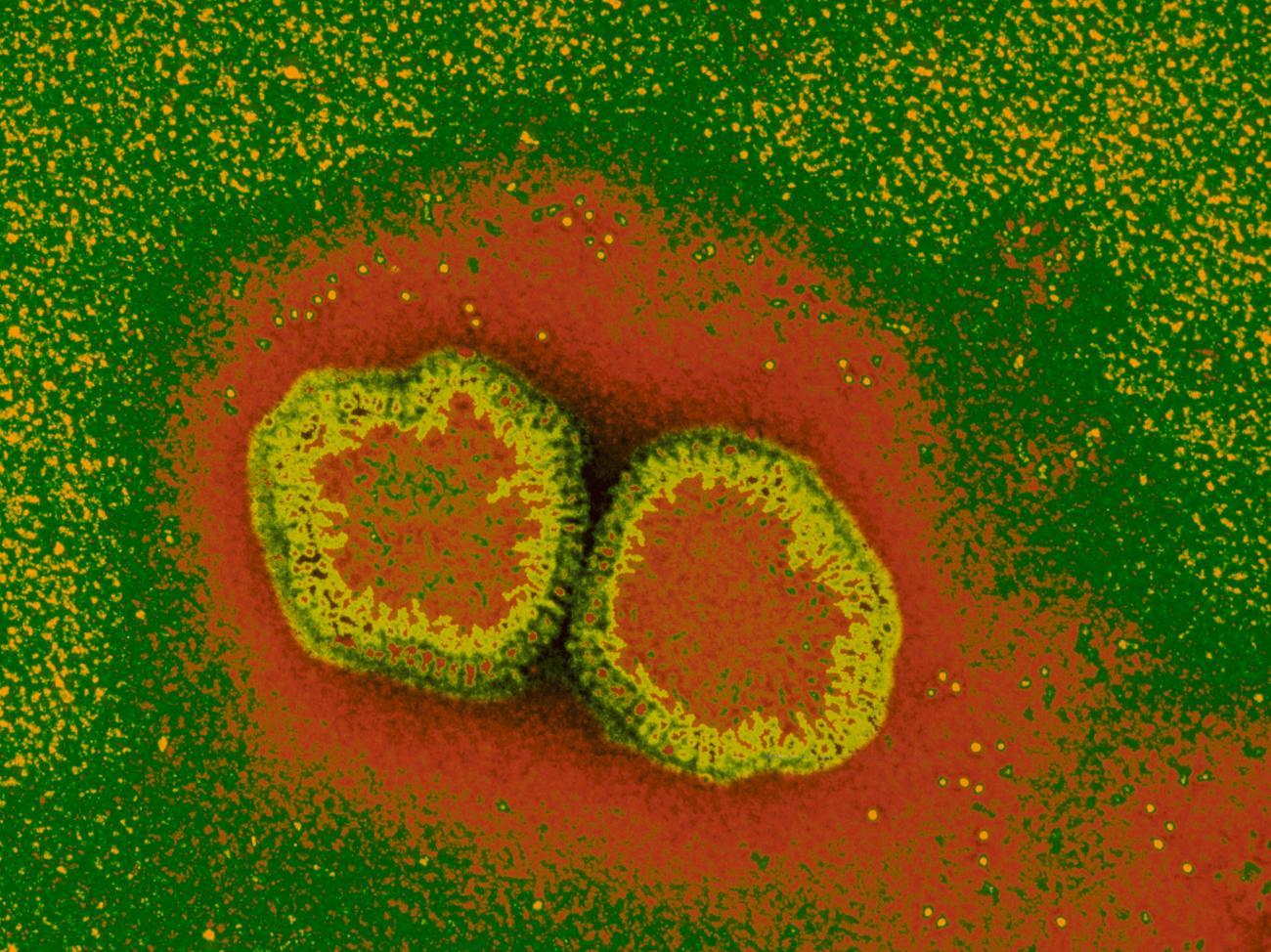
Keeping a close eye on influenza
In mainland France, influenza is monitored by the National Reference Center for Respiratory Viruses (Including Influenza), directed by Dr. Vincent Enouf at the Institut Pasteur, with the support of the 332 family physicians and pediatricians in the "Sentinelles" surveillance network, who take samples from patients with flu-like symptoms. "Every year we analyze an average of 2,000 samples for northern France. An associated laboratory in Lyon deals with the south of the country. We monitor these samples for influenza and other respiratory viruses," explains Vincent Enouf. "Any influenza viruses are examined and their genomes are sequenced to see how they are evolving and whether they still match the vaccine. Data from the RENAL hospital laboratory network (numbers of diagnoses and positive detections, etc.) for an extensive list of respiratory agents also show us what is circulating in hospitals and what impact it is having. Hospitals send us influenza virus strains from severe cases or occurrences of treatment failure so that we can analyze their sensitivity to antiviral drugs."
Every year we analyze an average of 2,000 samples for northern France. An associated laboratory in Lyon deals with the south of the country. We monitor these samples for influenza and other respiratory viruses.
Vincent EnoufHead of the National Reference Center for Respiratory Viruses (Including Influenza) at the Institut Pasteur
This virological surveillance is supervised by Santé publique France, which also monitors statistics such as the death rate from influenza and numbers of visits to hospital emergency departments or calls to the SOS Médecins medical emergency hotline. The national French strategy is part of a broader European approach – via the European Center for Disease Prevention and Control (ECDC) in Sweden and the EuroFlu network – coordinated by WHO/Europe, which in turn is linked with the international network of the World Health Organization: each country sends a selection of the seasonal viruses circulating within its borders to one of the five WHO Collaborating Centers (London, Atlanta, Melbourne, Tokyo and Beijing). Comparative analyses are carried out so that WHO can determine the composition of the following year's vaccine.* "With this approach, the emergence or spread of any new viral variants is immediately obvious, meaning that we can quickly sound the alert. When we see a virus that is out of the ordinary, we immediately send it to London."

Unfortunately we are unable to predict where and when the next outbreak will occur
How do new threats of disease outbreaks emerge?
There are three ways in which potential disease outbreaks can emerge. The first occurs when infectious agents cross the species barrier from animals to humans. This was the case for HIV, which jumped from chimpanzees to humans in the early 20th century, and the SARS virus, which in 2003 was transmitted from bats to masked palm civets – which in turn were eaten in restaurants serving exotic food in southern China and contaminated humans. Another way outbreaks can develop is when the genomes of pathogens change, leading to the emergence of "new" influenza viruses, for example, or to microbes becoming resistant to treatment – as we have seen with the resistance of the malaria parasite to antimalarial drugs and the resistance of bacteria to antibiotics. The third possibility is when viruses arrive in new geographical regions: the chikungunya virus, previously located in East Africa and India, affected Reunion Island in 2005; and the Zika virus, which had given rise to sporadic cases in Africa and South East Asia, reached the Pacific, with outbreaks in French Polynesia in 2013 and Latin America in 2015. These viruses which have spread from their habitat have since traveled to far-flung corners of the planet.
Can we predict the emergence of new threats so that we can avoid outbreaks?
Unfortunately we are unable to predict where and when the next outbreak will occur. We were expecting an influenza pandemic to originate in China, but the 2009 pandemic began in Mexico. We were surprised by the Ebola outbreak in West Africa in 2013-2014, because the virus had seemed to be limited to Central Africa. And no one would have predicted that camels in Saudi Arabia would be infected with a coronavirus which came out of nowhere!
What is the Institut Pasteur doing to tackle these threats?
If we are to have any hope of containing an outbreak as soon as it occurs, the important thing is being able to react extremely quickly. That is why we set up our Outbreak Investigation Task Force, which is ready at all times to send experts from the Institut Pasteur in Paris and the Institut Pasteur International Network to the field. These volunteers have a variety of skills to deal with potentially emerging pathogens, from avian influenza at the Institut Pasteur du Cambodge to hemorrhagic fevers in Senegal, plague in Madagascar and monkeypox in Bangui. There is no other institution in the world that is capable of responding to outbreaks not only by sending teams to the field but also by carrying out extensive basic and applied research on the subject.
Can you give us an example?
The Zika virus is a very good illustration. Since 2014, the institutes in the International Network have been working on this emerging virus. Entomologists have compared the vector capability of Aedes mosquitoes from several continents. My team has focused on demonstrating the role of the Zika virus in complications described in adults – Guillain-Barré syndrome – and children – microcephaly – during the outbreaks in Polynesia and the French West Indies. Basic research was performed on the virus structure, early immune reactions, passage across the placental barrier and neurological complications in infants, and more applied research looked into improving diagnostics and developing a vaccine. Since 2014, a total of more than 250 scientific articles on this virus have been published by Institut Pasteur scientists from 23 institutes in the International Network, consolidating the Institut Pasteur's position as a global leader in Zika virus research.






