The lowdown on meningitis, a public health challenge

On April 26, 2024, the World Health Organization held a high-level meeting at the Institut Pasteur to highlight the importance of tackling meningitis, a disease that comes in multiple, often severe forms, some of which can kill in the space of hours. It is crucial that we improve our knowledge of meningitis. What are the symptoms, and how can it be prevented? Vaccination is the solution, both to protect individuals and to tackle outbreaks at global level. In France, three forms of bacterial meningitis, which mainly affect children, are covered by vaccination.
Summary
Foreword - What are meningitis?
Key Figures - Acute bacterial meningitis
Symptoms - Spotting the signs as early as possible
News - A global road map to eradicate meningitis
Vaccine - New vaccine recommendation
Focus - The CNR, a source of biological expertise
Control and prevention - Find out more
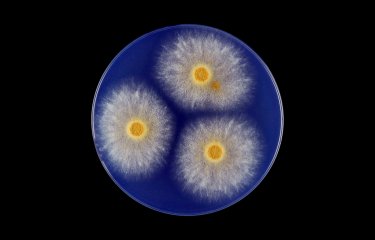
 Experimental Neisseria meningitidis bacteremia in mice. Neisseria meningitidis, also known as meningococcus or meningococcus. Copyright: Institut Pasteur.
Experimental Neisseria meningitidis bacteremia in mice. Neisseria meningitidis, also known as meningococcus or meningococcus. Copyright: Institut Pasteur.
Four years ago, the World Health Organization (WHO) adopted a road map aimed at "Defeating meningitis by 2030." And that was the focus of the high-level meeting held on April 26, 2024 at the Institut Pasteur. The event was hosted by the French government, represented by Frédéric Valletoux, Minister for Health and Prevention, and was held under the high patronage of the French President. It was an opportunity for the WHO Director-General and stakeholders involved in the global road map to hold discussions and highlight the importance of tackling what is still a deadly disease with major public health implications. Every year worldwide, 2.5 million people contract bacterial meningitis, including 500,000 cases of meningococcal meningitis.
Bacterial forms are the most severe
What is meningitis? Meningitis is an inflammation of the meninges, membranes that envelop the central nervous system (the brain and spinal cord). "This barrier is pretty strong – not much gets past it," explains Professor Muhamed-Kheir Taha, Head of the Invasive Bacterial Infections Unit and Director of the National Reference Center (CNR) for Meningococci at the Institut Pasteur. "But occasionally an external agent crosses the barrier and enters the space around the brain, generating an inflammatory reaction. This is meningitis." Infectious meningitis can be fungal (caused by a fungus), viral – the most frequent form and generally not serious –, or bacterial. Although bacterial meningitis is rarer than viral meningitis, it is severe and can be deadly. In 2023 in France, 560 cases of meningococcal meningitis and 59 deaths were recorded. In the first quarter of 2024, 180 people were affected.
Bacterial meningitis is a severe, rapidly progressing infection (see the Institut Pasteur disease fact sheet). It is unpredictable and can strike people at any age, even those in good health. "Acute bacterial meningitis begins very suddenly and develops rapidly. It can kill a person in excellent health in just a few hours." Rapid diagnosis is crucial so that it can be treated immediately, because in the absence of treatment it is invariably fatal. Even if treatment can be administered in optimal conditions, acute bacterial meningitis remains fatal for 10 to 15% of patients. Moreover, "a quarter of surviving patients suffer from debilitating after-effects that may include nervous system disorders, hearing loss and loss of kidney function. The burden on families, society and the economy is therefore very high." Recognizing the symptoms so that swift action can be taken is essential.
Spotting the signs as early as possible
Diagnosing meningitis is often a complex task. But there are signs to look out for, the most well known being sensitivity to light and a stiff neck. If you or someone in your care is experiencing these symptoms, you should seek medical care immediately. "The problem is that by the time these symptoms appear, the disease is already at an advanced stage. The first symptoms, which appear at an early stage, are non-specific," warns Professor Taha. "In the past 20 years, huge progress has been made in identifying early signs, and we teach doctors to be on the lookout for the early stages of meningitis. This is particularly important in the case of teenagers – if they complain of acute abdominal pain, the temptation, wrongly, is to presume that they have just had a heavy night out..."
In all cases, if red or purple blotches appear on the skin and do not fade when pressed, this is a sign of purpura, which can rapidly progress to purpura fulminans. In children with black skin, this prodromal symptom can be detected on the mucous membranes (for example the mouth). This symptom is a sign that urgent medical help is required: call the emergency services (dial 15 in France) or go to the nearest emergency department as quickly as possible.

Dr Muhamed-Kheir Taha
head of the Invasive Bacterial Infections Unit and Director of the National Reference Center (CNR) for Meningococci
In the past 20 years, huge progress has been made in identifying early signs, and we teach doctors to be on the lookout for the early stages of meningitis. This is particularly important in the case of teenagers – if they complain of acute abdominal pain, the temptation, wrongly, is to presume that they have just had a heavy night out...
Different symptoms at each stage
- Early signs (in the first few hours): high temperature, vomiting, headache. These symptoms are not specific to meningitis and may be confused with flu or gastroenteritis. Other signs may be mottled or blotchy skin, pain in the legs, stomach ache and diarrhea. Parents of young babies should be on the lookout for changes to their general behavior: "It is important to trust your instincts – if your child is not behaving in the usual way, this can be a warning sign," emphasizes Muhamed-Kheir Taha.
- Classic symptoms: sensitivity to light, headache, stiff neck, cold hands and feet, and projectile vomiting are symptoms that may appear at a later stage, although not necessarily all of them, and they may not occur in any particular order, which can be misleading, especially in infants (see graphic below).
 "Together against meningitis" collective.
"Together against meningitis" collective.
It is essential to treat bacterial meningitis quickly. The most aggressive forms (meningococcal and pneumococcal) progress very quickly and can result in death within 24 hours of the initial onset of symptoms. As soon as warning signs appear, medical care should be sought and medical staff should be notified of any changes in symptoms. A laboratory test is performed in hospital via a lumbar puncture. For cases of meningococcal meningitis, appropriate antibiotic treatment is administered to the patient and also to family members for preventive reasons. But as diagnosing meningitis is a complex process, vaccination plays a crucial part as it is the only means of prevention.
A global road map to eradicate meningitis
This is why WHO adopted the road map "Defeating meningitis by 2030" at the 73rd session of the World Health Assembly in 2020. The aim is to significantly reduce the number of cases of acute bacterial meningitis at global level to prevent further outbreaks. "Meningococcal meningitis is now rare in countries in the Global North. But countries in the Global South still experience severe outbreaks, with thousands of cases in the space of a few weeks," explains Muhamed-Kheir Taha.
For Professor Taha, a member of WHO's Technical Taskforce on Defeating Meningitis by 2030 and Head of the WHO Collaborating Center for Bacterial Meningitis, the goal of eradicating the most severe meningitis outbreaks is ambitious but achievable – "if we ensure that everyone has access to surveillance, diagnosis and treatment (by making drugs available to local populations). The same is true for prevention: countries need to hit hard by launching major vaccination campaigns." Such campaigns can have a rapid impact. In Sub-Saharan Africa, where meningitis is a major public health problem, there were hundreds of thousands of cases of group A meningococcal meningitis before vaccination was introduced in 2013. "From 2017 onwards no cases were detected, and there have been no more cases to this day!"
The meeting on April 26, 2024, the first high-level event organized in connection with the WHO program, was an opportunity for stakeholders to draw attention to challenges and commitments and also to raise funds, especially with the aim of boosting research. Three main priorities are currently driving the scientific community involved in meningitis research. The first is understanding why some bacteria cross the meningeal barrier. The second is elucidating why the inflammatory system reacts so strongly: "We are studying the body's reaction to understand why in some cases the inflammatory response is exaggerated and uncontrolled (cytokine storm). We think that this may be an avenue for action to help curb meningitis." Finally, it is crucial to continue developing new vaccines that target as many pathogens as possible.
New vaccine recommendation
The vaccines available in France today are those that target the strains circulating most widely in the country (see below). In France, the 11 compulsory vaccines for infants include three that target three of the four bacteria responsible for bacterial meningitis.
Which vaccines target which bacteria?
Here are the four bacteria mainly responsible for acute meningitis and the vaccines available in France:
- Neisseria meningitidis (meningococcus) // Vaccines against serogroups A, C, W, Y and serogroup B
- Streptococcus pneumoniae (pneumococcus) // Vaccine against 13 serotypes and soon against 20 of the most widespread serotypes
- Haemophilus influenzae // Vaccine against serotype B
 Researchers working in the Invasive Bacterial Infections unit, headed by Muhamed-Kheir Taha, at the Institut Pasteur. Copyright: Institut Pasteur/François Gardy
Researchers working in the Invasive Bacterial Infections unit, headed by Muhamed-Kheir Taha, at the Institut Pasteur. Copyright: Institut Pasteur/François Gardy
In France, meningococcal C vaccination is compulsory, but given the resurgence in cases caused by serogroups W and Y, the National Authority for Health (HAS) has proposed making the quadrivalent ACWY vaccine compulsory for all infants, instead of the meningococcal C vaccine, and it also recommends this vaccine for adolescents and young adults. Another recommendation is to make meningococcal B vaccination compulsory. In reaching these conclusions, the HAS referred to the research carried out by the National Reference Center (CNR) for Meningococci (see below) at the Institut Pasteur, led by Professor Taha. The CNR's research has also been made available to Santé publique France and to the Mathematical Modeling of Infectious Diseases Unit led by Simon Cauchemez at the Institut Pasteur; the latter unit is modeling the impact of the various vaccine strategies under consideration to inform the work of the HAS.
The new recommendations in France have come in response to a "post-COVID" resurgence. After the health measures introduced to tackle the COVID-19 outbreak were lifted, meningitis cases shot up. Compared with a total of 298 cases recorded between January and September 2019, 421 cases were recorded between January and September 2023 – a rise of 36%, even before the winter peak.
As Muhamed-Kheir Taha explains, "The meningococcal C vaccine is a good example of how effective compulsory vaccination is at improving population coverage. The meningococcal C vaccine was recommended in France in 2010 for all children aged one, with a catch-up vaccine possible up to the age of 24. Between 2010 and 2017, the vaccination strategy was not effective, and coverage in the 16-24 year age bracket remained insufficient. But the introduction of a dose at 5 months in 2017, followed by the imposition of compulsory vaccination in 2018, led to a drop in cases of this type of meningitis." The new compulsory vaccination measure is likely to come into force in a few months, and the impact will be monitored closely.
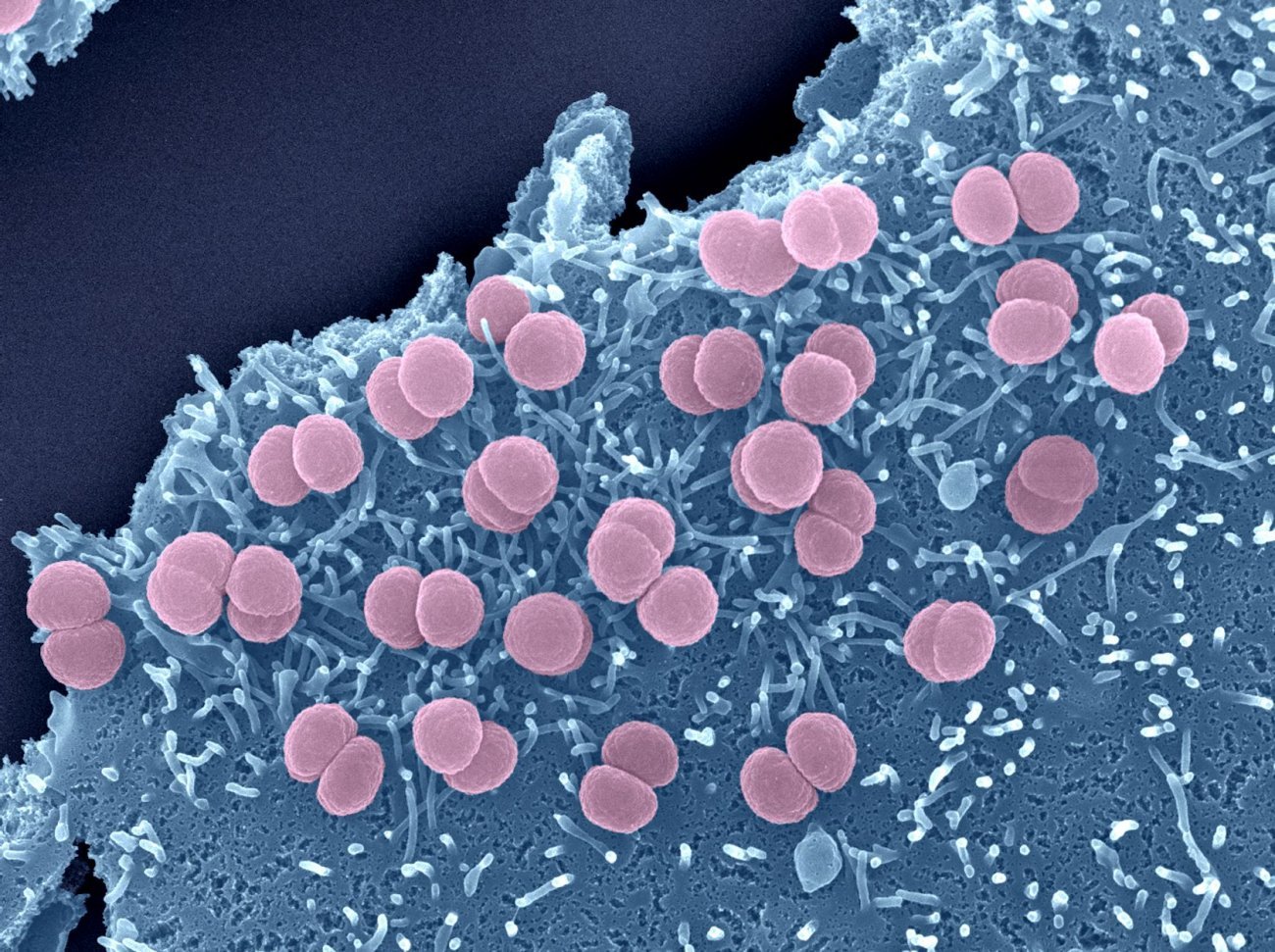
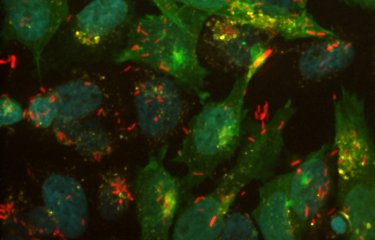
Neisseria meningitidis bacteria adhere to the surface of epithelial cells. Diplococci are entangled in microvilli of cellular origin.
Copyright: Institut Pasteur/Perrine Bomme, Plate-Forme Microscopie Ultrastructurale, Guillaume Duménil, INSERM U970, Paris Centre de Recherche Cardiovasculaire, HEGP - Colorization Jean-Marc Panaud.
The CNR, a source of biological expertise
The National Reference Center (CNR) for Meningococci at the Institut Pasteur offers biological expertise on meningococcal and Haemophilus influenzae meningitis in France. It performs epidemiological surveillance in collaboration with Santé publique France. In France, the CNR receives samples and strains from patients, which it analyzes to determine the strains involved (generally using whole-genome sequencing), and it also examines the antibiotic resistance of these strains. If novel clones or variants are identified, it sounds the alarm. The center is also actively involved in establishing vaccine strategies against invasive meningococcal infections in France.
Links to find out more
1. WHO and France convene high-level meeting to defeat meningitis
Global leaders highlight the need to defeat meningitis – a leading cause of disability – at a high-level meeting co-hosted by the World Health Organization (WHO) and Government of France, under the High Patronage of Emmanuel Macron, President of the French Republic. The event is taking place on 26-27 April 2024 at the Institut Pasteur and is supported by prominent athletes advocating on the cause ahead of the Paris Paralympics.
Read the press release ‘WHO and France convene high-level meeting to defeat meningitis’
2. The Vaccination Info Service website and its Meningitis and meningococcal septicaemia section | Vaccination Info Service (in French)
Please note that the new, more recent vaccination recommendations (described in this report) are not yet mentioned on this site.