An Institut Pasteur team has successfully developed a pentavalent vaccine against the five pathogenic arenaviruses circulating in South America and tested it in a primate model. Each of the viruses has a low incidence but a very high mortality rate, so combining them in a single vaccine would help facilitate vaccine development and ensure that the population can be protected as soon as possible.
New World arenaviruses, a family of viruses found in the Americas, can be highly pathogenic. The only existing vaccine targets the Junin virus, found in Argentina. There is no vaccine for the other viruses, since they currently have a low incidence in the human population. But sporadic emergences are becoming increasingly frequent and are reported with very high mortality rates. So "a multivalent vaccine seems the most appropriate way of offering a low-cost solution in the event of an outbreak, regardless of the virus responsible," explains Stéphanie Reynard, a research engineer in the Institut Pasteur's Biology of Viral Emerging Infections Unit. This is the type of vaccine that has been developed by the unit, hosted in the International Center for Infectiology Research (CIRI, CNRS/École normale supérieure de Lyon/Inserm/Claude Bernard Lyon 1 University), with the help of the Institut Pasteur's Bioinformatics Hub and the Inserm-Jean Mérieux BSL-4 laboratory.
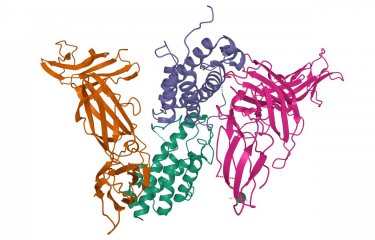
It all began with Lassa fever, a disease caused by an arenavirus that is endemic in West Africa and causes 5,000 to 6,000 deaths each year. In 2019, the research unit developed two vaccine candidates against the disease using live attenuated viruses to express Lassa virus antigens, the first based on the measles virus and the second on a virus known as Mopeia, which is closely related to Lassa virus but not pathogenic for humans. Although it was the measles virus vaccine that was selected for a clinical trial, the Mopeia virus proof of concept was particularly interesting: "Infection with this modified attenuated virus generated a very strong immune response in an in vitro model. It is also possible to replace the Mopeia virus glycoprotein gene with any of the glycoprotein genes from viruses in the same family, arenaviruses. Glycoproteins are involved in viral entry into the cell at the point of infection and therefore represent a major target for the immune system," explains Stéphanie Reynard.
Adapting the MOPEVAC vaccine to New World arenaviruses
So the team adapted this vaccine candidate, known as MOPEVAC, to the five arenaviruses circulating in South America that are dangerous for humans. "We started with a proof of concept: a monovalent vaccine targeting just one of these viruses, Machupo. We then developed the pentavalent vaccine, which we tested against the Machupo virus to make sure that it offered the same level of protection, and against the Guanarito virus to demonstrate that it was effective against a second virus," explains Sylvain Baize, Head of the Biology of Viral Emerging Infections Unit.
These experiments, which were made possible by internal funding from the Institut Pasteur, demonstrated that the vaccine is highly effective, since it induced sterilizing immunity in animal models, in other words preventing the virus from replicating so that it is brought under control immediately after infection. In 2023, the team will test the pentavalent vaccine against the other three viruses and against another closely related virus that has emerged in North America but has not been included in the vaccine formulation. The program, funded by the French government in connection with the French national recovery plan and the Investing in the Future program, will thereby determine whether the protection offered by the vaccine may also be extended to emerging viruses.
Source:
A MOPEVAC multivalent vaccine induces sterile protection against New World Arenaviruses in non-human primates, Nature Microbiology, January 05, 2023
Stéphanie Reynard1,2, Xavier Carnec1,2, Caroline Picard1,2, Virginie Borges-Cardoso1,2, Alexandra
Journeaux1,2, Mathieu Mateo1,2, Clara Germain1,2, Jimmy Hortion1,2, Laure Albrecht1,2, Emeline Perthame3, Natalia Pietrosemoli3, Audrey Vallvé4, Stéphane Barron4, Aurélie Duthey4, Orianne Lacroix4, Ophélie Jourjon4, Marie Moroso4, Lyne Fellmann5, Pierre-Henri Moreau5, Maïlys Daniau6, Catherine Legras-Lachuer6, Manon Dirheimer7, Caroline Carbonnelle4, Hervé Raoul4, and Sylvain Baize1,2
1- Biology of Viral Emerging Infections Unit, Institut Pasteur, Lyon, France.
2- CIRI, International Center for Infectiology Research, Univ Lyon, Inserm, U1111, Claude Bernard Lyon 1 University, CNRS, UMR5308, ENS de Lyon, F-69007, Lyon, France.
3- Institut Pasteur, Université de Paris, Bioinformatics and Biostatistics Hub, Paris, F-75015, France.
4- Inserm-Jean Mérieux BSL-4 laboratory, Inserm US003, 69007 Lyon, France.
5- SILABE, University of Strasbourg, Fort Foch, 67207 Niederhausbergen, France.
6- ViroScan3D SAS, Trevoux, France.
7- Inserm, Auvergne Rhône-Alpes regional delegation, Bron, France.