Infection-related cancer

More than one in six cases of cancer worldwide are caused by infection. In total, some 2.2 million new cancer cases every year are believed to be the result of infection by a pathogenic agent. Eight viruses, one bacterium and three parasites have been classified as group 1 carcinogens (known to be carcinogenic to humans) by the International Agency for Research on Cancer, a division of the World Health Organization.
These include the hepatitis B and hepatitis C viruses, which can lead to chronic infections and liver cancer and claim more than a million lives each year. The Helicobacter pylori bacterium is responsible for the majority of cases of stomach cancer, the second leading cause of cancer death worldwide. Infection by some forms of papillomavirus is associated with cervical cancer, the fourth leading cause of cancer death in women. HIV is also classified as a carcinogen, since the immunodeficiency it induces increases the risk of cancer.
Parasites – the first suspect
Suspicions that infectious agents were involved in cancer emerged in the late 19th century and focused at that time on parasites, especially Schistosoma, the flatworms responsible for schistosomiasis, a disease prevalent in tropical and subtropical regions. Chronic infection with Schistosoma can lead to bladder cancer, but it took 50 years to establish proof of the parasite's role. We now know of three parasites that can lead to cancer: Schistosoma and two other parasitic worms, one endemic in some South-East Asian countries (including Thailand, Laos, Vietnam and Cambodia) and the other in the Far East, both associated with gall bladder and biliary tract cancer.
Epstein-Barr – the first virus implicated
The second major milestone in the history of infection-related cancer took place in 1958, when British surgeon Denis Burkitt described a lymphoma (since renamed "Burkitt's lymphoma") that was affecting children in Equatorial Africa, and put forward the theory that this cancer was caused by infection. In 1964, fellow Briton Michael Epstein discovered viral particles in cells cultured from these lymphomas. It was demonstrated in the early 1970s that the "Epstein-Barr" virus was indeed responsible for Burkitt's lymphoma. This virus, which can actually be found in nearly all individuals – fortunately most often with no consequences – is also linked to the development of nasopharyngeal carcinoma. It was the first virus to be officially identified for its role in the onset of human cancer.
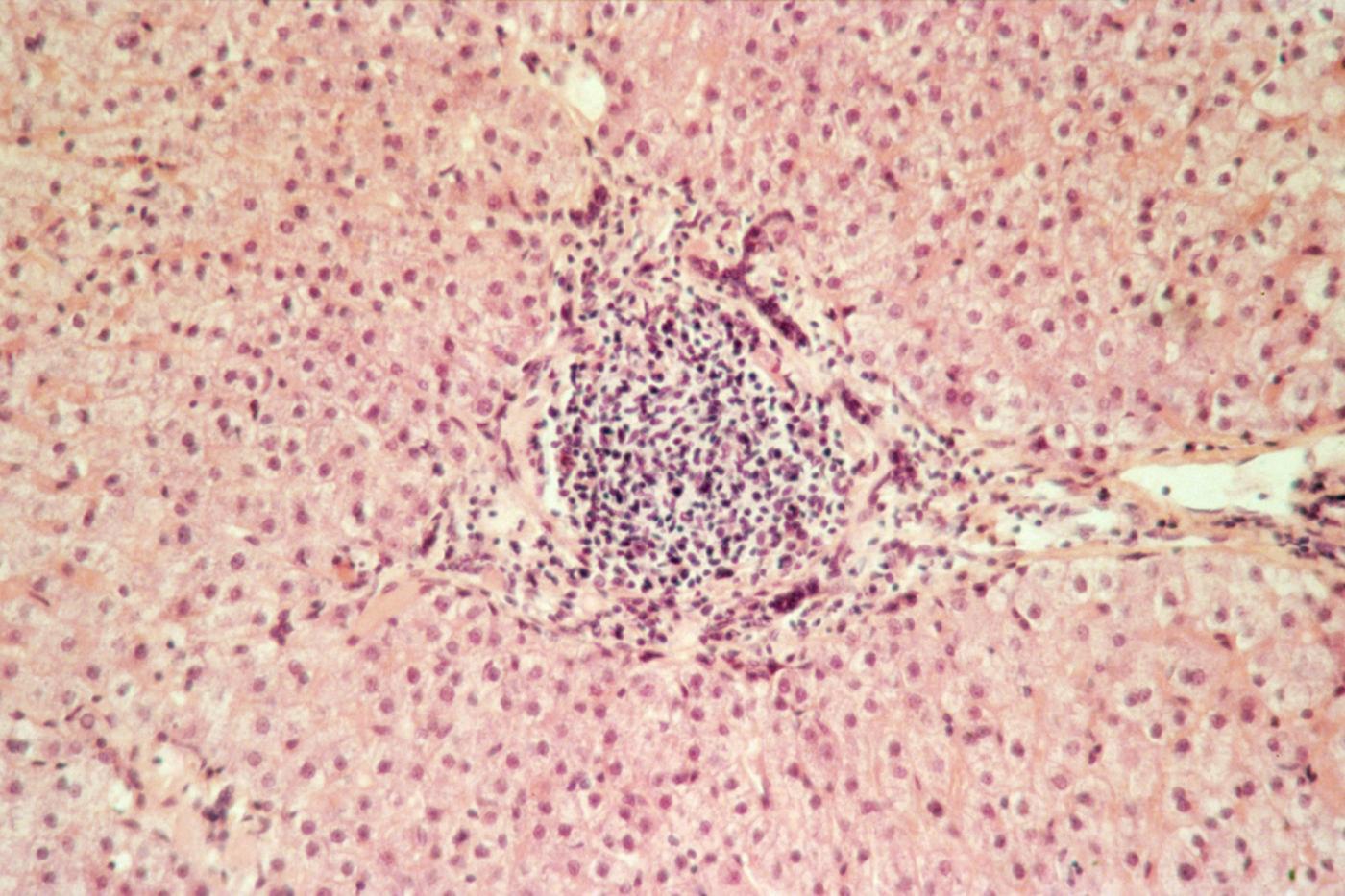
Above: histological section of liver of patient with hepatitis C. Chronic hepatitis C can cause cirrhosis and liver cancer. © Institut Pasteur
New treatments and biomarkers
There are 700,000 new cases of liver cancer worldwide every year. "While the majority of these cancers are infection-related, we should point out that in industrialized countries, the main cause is alcoholic cirrhosis," notes Prof. Stanislas Pol, Head of the Immunobiology of Dendritic Cells Unit and the Center for Translational Science at the Institut Pasteur, and Head of the Hepatology Department at Cochin Hospital. Regardless of the cause, liver cancer is difficult to treat; it has become the main reason for liver transplants in France. Research for more effective treatments is vitally important. "We are currently working together with La Pitié Salpétrière Hospital on an immunotherapy trial in liver cancer patients, using a molecule known as sitagliptin, with the aim of reducing the size of tumors," explains Stanislas Pol, whose research has already resulted in significant progress in treating viral hepatitis.
Another challenge is the early detection of liver cancer. Pascal Pineau, from the Nuclear Organization and Oncogenesis Unit led by Anne Dejean, is investigating the specific characteristics of liver cancer in different regions across the world, based on the genetic disturbances caused by viral hepatitis in the hepatocytes of cancer patients. One of the goals of his work is to identify biomarkers for the early stages of liver cancer. He is currently studying liver biopsies and blood samples from hundreds of African patients, with the members of the Institut Pasteur International Network (Pasteur Center in Cameroon and the Institut Pasteur in the Central African Republic.) "The problem is that liver cancer varies hugely from one geographic region to the next," notes the scientist. "We need to find a panel of biomarkers. We are still at the very beginning of our search."
Potentially avoidable cancer
In the 1970s, the potential carcinogenic effect of several other viruses was confirmed: the hepatitis B virus, suspected since the 1950s of being linked to liver cancer; a retrovirus associated with a rare form of leukemia (HTLV-1 ), and several types of papillomavirus responsible for cervical cancer. Then came proof of the role of Helicobacter pylori, the only bacterium – even if others are currently under suspicion – to be classified as a group 1 carcinogen, since 1994. That same year, another cancer-causing virus was discovered: herpesvirus 8, responsible for Kaposi's sarcoma – a cancer sadly made famous by the AIDS epidemic but which also affects HIV-negative individuals in Africa. The latest infectious agent to be added to the infamous group 1 is a relatively rare virus identified in 2008, Merkel cell polyomavirus, which is linked to a very aggressive form of skin cancer.
These forms of cancer linked to pathogens all have one thing in common: they can be avoided if the causative infection can be prevented or treated in time. A major breakthrough was made in this respect in the 1980s concerning hepatitis B and liver cancer.

Preventing or treating the infection means eliminating the risk of cancer.
What is the incidence of infection-related cancer worldwide today?
Around 30 to 50% of the 14 million cases of cancer that occur worldwide each year can be avoided. There are those caused by smoking, alcohol, pesticides and other toxic chemicals, and then there are those caused by infectious agents, which are responsible for more than 15% of cancer cases, with considerable disparities from one world region to the next. In western countries, estimates suggest that fewer than 10% of cancer cases are caused by infection, although that still represents a huge number. In developing countries, however, the figure is much higher, in the region of 30%. If we take the example of India, home to nearly a fifth of the world's population, one in every four global cases of cervical cancer occur in the country. Another characteristic of infection-related cancers is that they generally strike at an earlier age than other forms of cancer. For some cancer-causing pathogens, one risk factor that increases the chances of tumor development is being infected at a very early age or as a baby. This is the case for hepatitis B and liver cancer, which can affect young adults.
How do these pathogens cause cancer?
They work in different ways. Several types of HPV, HTLV-1, the Epstein-Barr virus and herpesvirus 8 are all "direct" oncogenic viruses, for example producing proteins that trigger changes in cells. Then there are "indirect" oncogenic viruses, which either cause inflammation that eventually results in cancer – this is the case with the hepatitis B and C viruses, the H. pylori bacterium and cancer-causing parasites –, or lead to immunosuppression, as with HIV. Most cases of cancer linked to HIV are actually caused by direct oncogenic viruses such as the Epstein-Barr virus, herpesvirus 8 or HPVs, against which the body is no longer able to defend itself.
So infection by a carcinogen does not systematically lead to cancer?
Not at all. Infection-related cancer only occurs in a small proportion of those infected. The extreme example of this is the Epstein-Barr virus – virtually all the world's population is infected by this virus, but only a few hundred thousand actually go on to develop tumors. So despite the frequency of the virus, it rarely leads to cancer. The risk varies depending on the carcinogenic infectious agent, but in general only a small proportion of those infected develop cancer. In other words, the infectious agent alone does not lead to cancer, although it needs to be there for the cancer to occur. This means that there are cofactors – other risk factors also have a part to play.
How does knowing which infectious agent is responsible help us to combat cancer?
It means that we are able to study the mechanisms involved so that we can understand them better and identify potential molecular targets. In practice, the major breakthrough has been vaccination, which is now possible for hepatitis B and some types of HPV. Preventing or treating the infection means eliminating the risk of cancer. There are other preventive methods as well as vaccination. HTLV-1, for example – a virus that we study extensively in my laboratory – is linked with an extremely severe form of leukemia, with an average prognosis of just six months for acute forms, which develops in individuals who acquire the virus at a very early age. In socio-economically developed regions and countries where this leukemia is endemic – the West Indies, French Guiana, Brazil and Japan, for example – screening of pregnant women has been introduced. Women who are infected are advised to avoid breastfeeding. This means that one of the very worst forms of cancer can be avoided.
The first cancer vaccine

In 1981, a study carried out in Taiwan, where hepatitis B was highly prevalent, demonstrated that carriers of this virus (usually passed on by mother-to-child transmission, but also via the bloodstream or through sexual intercourse) were 200 times more likely than other individuals to develop liver cancer. This led to a significant turning point: a hepatitis B vaccine, designed at the Institut Pasteur (see inset) and easy to produce at industrial scale, was introduced in 1985. Vaccination soon became widespread in several countries across the world, drastically reducing the incidence of infection and related complications including cirrhosis and liver cancer. Tens of millions of individuals worldwide have now been vaccinated, and millions of cases of cancer avoided. The hepatitis B vaccine was the first example of a vaccine capable of preventing cancer.
Hepatitis B: from preventative to curative vaccine
The current preventive vaccine for hepatitis B was developed at the Institut Pasteur by the team led by Professor Pierre Tiollais. This vaccine, available since 1985, is 95% effective and is now systematically given to infants or adolescents in around 200 countries. According to the World Health Organization, "over 1 billion doses of hepatitis B vaccine have been used worldwide. In many countries where between 8-15% of children used to become chronically infected with the hepatitis B virus, vaccination has reduced the rate of chronic infection to less than 1% among immunized children."

However, 250 million individuals worldwide are already chronic carriers of the virus. "This is a major public health challenge," stresses Maryline Bourgine, a member of the Institut Pasteur's Molecular Virology and Vaccinology Unit, directed by Pierre Charneau. "We are working to develop a therapeutic vaccine candidate for these chronic carriers*. The idea is to induce an immune reaction in the patient that will tackle and eliminate the virus. We have high hopes for this strategy since the most effective antiviral drugs currently do not actually eliminate the virus from the livers of chronic carriers. We are working on several vaccine candidates based on an innovative technique developed in this laboratory. The first results of the efficacy tests are expected in the next few months."
*In connection with the Institut Pasteur's Major Federating Program on Vaccinology.
A second cancer vaccine
Around 20 years later, in 2007, a second "cancer vaccine" became available, targeting the forms of papillomavirus most frequently linked to cervical cancer. In more than 60% of cases, this vaccine prevents the onset of cervical cancer, the second most common type of cancer in women at global level, which claims more than a thousand lives each year in France.

The human papillomaviruses (HPVs) involved in genital cancers are sexually transmitted, and just two of them (HPV-16 and HPV-18) – both covered by the two available vaccines – are responsible for 70% of cases. These HPVs are particularly widespread, and in France it is recommended that girls should be vaccinated before they become sexually active, between the ages of 11 and 14. A catch-up vaccination can be administered up to the age of 20. The impact of this vaccination is being closely monitored (see inset).
Cervical cancer: monitoring the impact of vaccination
Around 20 "high-risk" human papillomaviruses (HPVs) can result in genital cancer. These sexually-transmitted viruses can cause benign lesions such as genital warts, or malignant lesions that can develop into cervical cancer over a period of 15 to 20 years. Since 2007, girls have been offered vaccination against the two types of HPV mostly responsible for cervical cancer.

The Institut Pasteur's Pharmacoepidemiology and Infectious Diseases Unit, directed by Didier Guillemot, is carrying out a study on 1,000 young women from a cohort of students to assess the impact of vaccination on the circulation of these different viruses in the population. To what extent does vaccination lower the frequency of the two main viruses (HPV-16 and HPV-18) in young women? If vaccination leads to a drop in these HPVs, will other rarer HPVs eventually gain the upper hand? This post-vaccine study will provide important answers that will help us anticipate the effect of the vaccination and propose suitable public health initiatives.
Treatment to eliminate carcinogens
The two vaccines mentioned above are currently the only available vaccines that can be used to prevent cancer. In the absence of vaccine prevention, the alternative approach to avoid infection-related cancer is to treat the infection early enough – bearing in mind that it takes at least ten years from the acquisition of a pathogenic agent to the development of cancer.
Some examples of treatment include antibiotics that can entirely eradicate the Helicobacter pylori bacterium, which currently infects half the world's population and can lead to stomach cancer. The latest generation of hepatitis C treatments permanently eliminates the virus in its chronic carriers – there are millions of these carriers worldwide (see inset). Although the widespread use of these treatments in developing countries is limited by their high cost, they have the potential to prevent hundreds of thousands of cases of liver cancer in the future.
A rapid diagnostic test
Estimates suggest that 150 million people in the world are chronically infected by the hepatitis C virus. "Most of them don't actually know that they are infected," points out Darragh Duffy, a member of the Institut Pasteur's Immunobiology of Dendritic Cells Unit. This scientist was involved in a three-year European program* that led to a mobile rapid diagnostic test for the virus. "Given the time required to transport patient samples to a laboratory and to perform traditional analysis methods, it sometimes takes one to two weeks to establish a diagnosis. The test that we developed with the company Epistem can be used at the patient's bedside and provides a result within an hour. This means that patients needing treatment can be easily identified and given one of the many effective medications now available. We are currently presenting the test to medical humanitarian NGOs working at the front line in the field."
*PoC HCV, coordinated by Matthew Albert, former Head of the Institut Pasteur's Immunobiology of Dendritic Cells Unit, under the aegis of Inserm.

While scientific research has led to major progress in tackling several infection-related cancers, the task ahead is still a daunting one. No fewer than 250 million people worldwide are already chronically infected by the hepatitis B virus, and there are no available treatments that can eliminate the virus from their body (see inset).
The eradication of the H. pylori bacterium using antibiotics, a promising approach to stomach cancer prevention, is seriously under threat as a result of the development of antibiotic resistance (see opposite). Solutions will depend on the answers to myriad questions currently under study in laboratories: what intricate mechanisms do these infectious agents use to induce cancer? How do our bodies react to these pathogens? Why do some infected people develop cancer but not others?
Helicobacter pylori: from therapeutic targets to stomach cancer markers
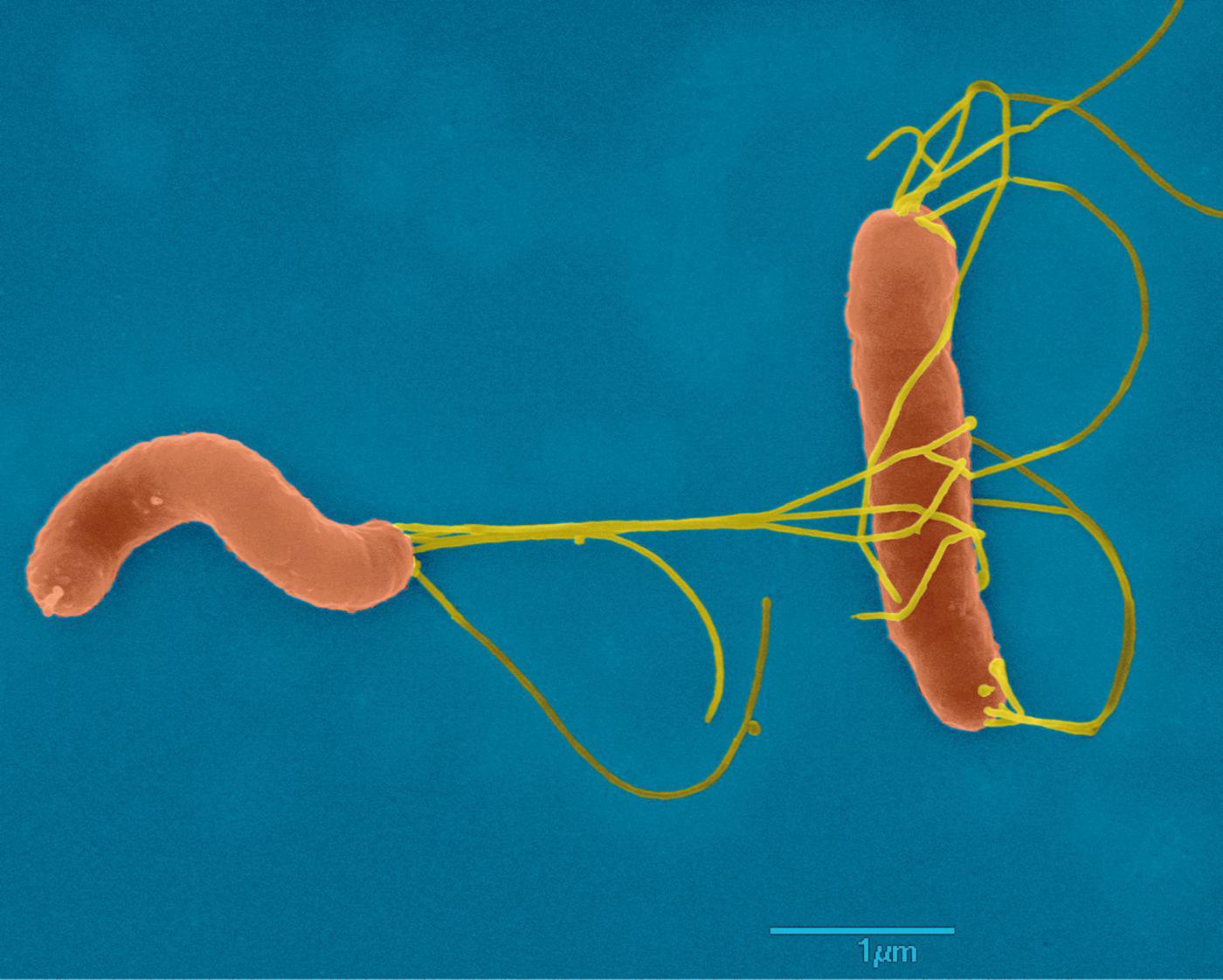
"Helicobacter pylori is the only bacterium capable of proliferating in the acidic environment of the stomach. It infects 50% of the world's population and can lead to peptic ulcers, chronic gastritis and, in 1 to 3% of cases, stomach cancer," explains Hilde De Reuse, Head of the Institut Pasteur's Helicobacter Pathogenesis Unit. "We are working to shed light on the molecular mechanisms that enable Helicobacter pylori to survive in the hostile environment of the stomach and to remain there for years, causing lesions. By deciphering these mechanisms, we have identified new therapeutic targets, especially a nickel transporter that is essential for the activity of urease, an enzyme required by the bacterium to colonize the stomach." Finding targets for future drugs is becoming increasingly crucial, since although antibiotic treatment can be used to eradicate the bacteria in most infected individuals, the efficacy of this treatment is threatened by the growing antibiotic resistance of H. pylori.
In the same laboratory, recent work has raised hopes for the possibility of early diagnosis of stomach cancer, which is responsible for 800,000 deaths worldwide each year. "We are examining host factors associated with the pathogenesis of the infection," explains Eliette Touati. "By working in collaboration with institutes in the Institut Pasteur International Network, we have been able to analyze a large number of patients suffering from gastritis and stomach cancer. This research has revealed two potential 'biomarkers' that can be detected in the blood. Our aim is to combine several biomarkers that signal very early-stage stomach cancer, so that we can identify those at risk." These individuals could be treated early on with antibiotics to eliminate H. pylori infection in hopes of stopping the cancer from developing. Using biomarkers may also increase the chances of recovery in patients already suffering from cancerous lesions.