Before the vaccine era, diphtheria was the most deadly respiratory infection in young children. There are still outbreaks of diphtheria in some world regions and cases can occur among unvaccinated individuals, with severe consequences. Antibiotics are vital in treating diphtheria, and the emergence of antibiotic resistance is a major public health concern. A team of Institut Pasteur scientists has identified the origins of penicillin resistance in the bacterial agent responsible for diphtheria.
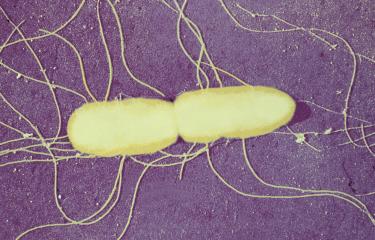
Thanks to the vaccine developed in the 1920s by Gaston Ramon (page in French), a veterinarian and biologist at the Institut Pasteur, diphtheria has virtually disappeared in industrialized countries and many other world regions. But the bacterial infectious agent, Corynebacterium diphtheriae (C. diphtheriae), is still transmitted among the human population, and can cause infection in unvaccinated individuals. If there is insufficient vaccine coverage, as is the case in some crisis-hit regions, outbreaks can soon occur.
The critical role of antibiotics in treating diphtheria
Treatment for diphtheria involves administering an antitoxin serum and/or a course of antibiotics as soon as possible. But production of the antitoxin serum has virtually stopped at global level. "Antibiotic treatment is crucial for infected individuals and people they are in contact with. Penicillin, one of the first antibiotics to be brought to market, is often still used to treat diphtheria," explains Sylvain Brisse, Head of the Biodiversity and Epidemiology of Bacterial Pathogens Unit and Head of the National Reference Center (CNR) for Corynebacteria of the Diphtheriae Complex.
Research into penicillin resistance in diphtheria using CNR strains
Resistance to penicillin is currently emerging in the diphtheria agent. Sylvain Brisse's team set out to determine the rate of resistance to penicillin and to understand the origins of resistance in strains of the agent detected in France. "The task of the National Reference Center for Corynebacteria of the Diphtheriae Complex, set up in 2000 following a major diphtheria outbreak in the former USSR, is to collect and characterize strains of C. diphtheriae. The strains collected in mainland France and French overseas territories between 2008 and 2017 were characterized for their sensitivity to 19 antibiotics, including penicillin, and their whole genome sequence was determined," explains Sylvain Brisse.
Discovery of a resistance gene
Resistance to penicillin was detected in 17% of strains, and multiple resistance (the resistance of a single bacterium to several antibiotics) was observed. A variant of a gene associated with a low affinity for penicillin was discovered, which explains why bacteria with the variant are resistant to the effect of the antibiotic. The gene was found in a variety of genetic lineages of C. diphtheriae, indicating that it can also be transmitted to new lineages. It is sometimes carried by a plasmid, a bacterial genetic element known to carry multiple resistance genes. The plasmid here was newly described in this study. Finally, the authors demonstrated that the gene confers resistance not only to penicillin, but also to several other antibiotics in the same family.
These results provide a current snapshot of antibiotic resistance in the diphtheria agent and reveal a new penicillin resistance gene in this pathogen. The findings will help refine the choice of antibiotics used to treat patients and improve diagnosis of antibiotic resistance in diphtheria. More generally, the work carried out by the National Reference Center and its host research unit will provide us with a greater understanding of the re-emergence and spread of diphtheria.
Source:
Population genomics and antimicrobial resistance in Corynebacterium diphtheriae, Genome Medicine, November 27, 2020
Melanie Hennart1,2, Leonardo G. Panunzi1,3, Carla Rodrigues1, Quentin Gaday4, Sarah L. Baines5, Marina Barros-Pinkelnig1, Annick Carmi-Leroy1,6, Melody Dazas1,6, Anne-Marie Wehenkel4, Xavier Didelot7, Julie Toubiana1,6,8, Edgar Badell1,6 and Sylvain Brisse1,6
1Biodiversity and Epidemiology of Bacterial Pathogens, Institut Pasteur, Paris, France
2Collège doctoral, Sorbonne Université, F-75005 Paris, France.
3Institut Français de Bioinformatique, CNRS UMS 3601, Evry, France.
4Unité de Microbiologie Structurale, Institut Pasteur, CNRS UMR 3528, Université de Paris, F-75015 Paris, France.
5Doherty Applied Microbial Genomics, Department of Microbiology & Immunology, The University of Melbourne at The Peter Doherty Institute for Infection & Immunity, Melbourne, Victoria, Australia.
6Institut Pasteur, National Reference Center for Corynebacteria of the Diphtheriae Complex, Paris, France.
7School of Life Sciences and Department of Statistics, University of Warwick, Coventry, UK. 8Department of General Pediatrics and Pediatric Infectious Diseases, Hôpital Necker-Enfants Malades, APHP, Université de Paris, Paris, France.
This study is part of the priority scientific area Antimicrobial Resistance of the Institut Pasteur's strategic plan for 2019-2023.