Depression is a complex multifactorial condition whose underlying mechanisms have still not been elucidated. Available treatments are therefore far from effective, and it is estimated that 30% of patients are resistant to conventional treatment. Scientists from the Institut Pasteur, in collaboration with teams from Sainte-Anne Hospital, have shed light on the role of brain inflammation as a mechanism that may lead to depression. This is an important discovery in our understanding of the condition, paving the way for new treatment possibilities.
According to WHO, depression is the leading cause of disability worldwide, with major consequences for individuals and a high cost for society. Current antidepressant medications, which mainly target three molecules – serotonin, noradrenaline and dopamine –, are only partially effective, with a remission rate of less than 65%. In recent years, an anesthetic agent, ketamine, has been the focus of considerable research. This molecule is often used to reduce pain and limit the consumption of post-operative opioids.
Clinical trials have demonstrated rapid, spectacular clinical efficacy in patients with treatment-resistant depression. "A major therapeutic revolution is under way: now the aim is to understand the mechanisms at work and to develop new treatments which target those mechanisms," explains Fabrice Chrétien, Head of the Experimental Neuropathology laboratory at the Institut Pasteur.
Ketamine: hopes for future treatments
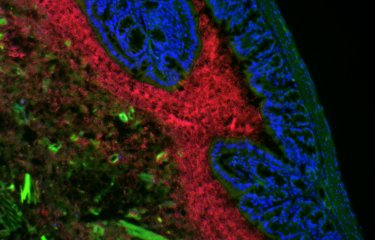
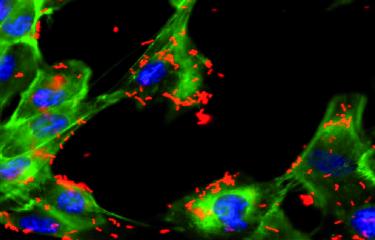
Following a translational research effort involving the Institut Pasteur and the Psychiatry and Neuroscience GHU (a consortium of teaching hospitals in Paris), the teams led by Professor Chrétien at the Institut Pasteur and Professor Gaillard at Sainte-Anne Hospital revealed a new mechanism of action of ketamine. In a murine model of induced depression, they showed that ketamine modulated the activation of microglial cells, immune cells in the brain that act like a "police force" by producing inflammatory and neurotoxic substances when activated.
By taking blood samples from patients with treatment-resistant depression who were given ketamine, the scientists also revealed a peripheral biomarker of ketamine efficacy that can be used to characterize patients who will benefit most from treatment.
"These data both confirm the key role of neuroinflammation in the pathophysiology of depression and pave the way for a personalized medicine approach, giving patients who will be most receptive to a future treatment the opportunity to benefit from it," concludes Fabrice Chrétien.
Source
Microglial production of quinolinic acid as a target and a biomarker of the antidepressant effect of ketamine, Brain, Behaviour and Immunity, 28 juin 2109
Franck Verdonka,b,c, Anne-Cécile Petita,d,e, Pierre Abdel-Ahadd,e,f, Fabien Vinckierd,e,f,Gregory Jouviona, Pierre de Maricourtd,e,f, Gabriela Ferreira De Medeirosa, Anne Danckaerta,g, Juliette Van Steenwinckelh,i, Michael Blatzera, Anna Maignanj, Olivier Langerona,c,k, Tarek Sharshara,e,l, Jacques Callebertm, Jean-Marie Launaym, Fabrice Chrétiena,e,n, Raphael Gaillarda,d,e
a Institut Pasteur, Experimental Neuropathology Unit, Infection and Epidemiology Department, Paris, France
b Department of Anaesthesiology and Intensive Care, Saint Antoine Hospital, Assistance Publique-Hôpitaux de Paris, Paris, France
c Sorbonne University, Paris, France
d Service Hospitalo Universitaire, Centre Hospitalier Sainte-Anne, Paris, France
e Paris Descartes University, Sorbonne Paris Cité, Paris, France
f Inserm, Laboratoire de “Physiopathologie des maladies Psychiatriques”, Centre de psychiatrie et neurosciences, CPN U894, Institut de psychiatrie (GDR 3557), Paris, France
g Institut Pasteur, UtechS Photonic BioImaging (Imagopole) – C2RT, Paris, France
h Inserm, U1141 Paris, France
i Paris Diderot University, Sorbonne Paris Cité UMRS 1141, F-75019 Paris, France
j Service Universitaire de Psychiatrie d'adultes, Centre Hospitalier de Versailles, Le Chesnay, France
k Multidisciplinary Intensive Care Unit, Department of Anesthesiology and Critical Care, La Pitié-Salpêtrière Hospital, Assistance Publique-Hôpitaux de Paris, Paris, France
l Department of Intensive Care, Centre Hospitalier Sainte Anne, Paris, France
m Service de Biochimie et Biologie Moléculaire, INSERM U942, Hôpital Lariboisière, Assistance Publique-Hôpitaux de Paris, Paris, France
n Laboratoire hospitalo-universitaire de Neuropathologie, Centre Hospitalier Sainte Anne, Paris, France
This study is part of the priority scientific area Brain connectivity and neurodegenerative diseases of the Institut Pasteur's strategic plan for 2019-2023.