The human body is inhabited by billions of symbiotic bacteria, carrying a diversity that is unique to each individual. The microbiota is involved in many mechanisms, including digestion, vitamin synthesis and host defense. It is well established that a loss of bacterial symbionts promotes the development of allergies. Scientists at the Institut Pasteur have succeeded in explaining this phenomenon, and demonstrate how the microbiota acts on the balance of the immune system: the presence of microbes specifically blocks the immune cells responsible for triggering allergies. These results are published in Science.

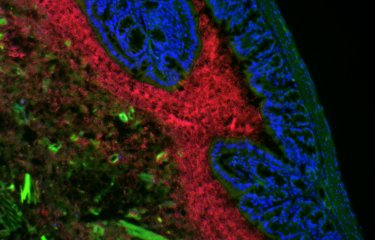
A cluster of type 3 cells (shown in green) in a mouse colon. These cells are induced by the microbiota and block type 2 allergic reactions. © Institut Pasteur
The hygiene hypothesis[1] suggests a link between the decline in infectious diseases and the increase in allergic diseases in industrialized countries. Improvements in hygiene levels necessarily lead to reduced contact with microbes that is paralleled by an increased incidence in allergic and autoimmune diseases, such as type 1 diabetes.
Epidemiological studies have substantiated this hypothesis, by showing that children living in contact with farm animals – and therefore with more microbial agents – develop fewer allergies during their lifetime. Conversely, experimental studies have shown that administering antibiotics to mice within the first days of life results in a loss of microbiota, and subsequently, in an increased incidence in allergy.
However, until now, the biological mechanisms underlying this phenomenon remained unclear. In this study published in Science, the team led by Gérard Eberl (head of the Microenvironment and Immunity Unit at the Institut Pasteur) shows that, in mice, symbiotic intestinal microbes act on the immune system by blocking allergic reactions.
Several types of immune response can be generated in order to defend the organism. The presence of bacterial or fungal microbes provokes a response from immune cells known as type 3 cells. These immune cells coordinate the phagocytosis and killing of the microbes. However, in the case of infection by pathogenic agents that are too large to be handled by type 3 cells (such as parasitic worms and certain allergens), the cells that organize the elimination of the pathogen, but also allergic reactions, are known as type 2 cells.
In this study, scientists at the Institut Pasteur have shown that type 3 cells activated during a microbial aggression act directly on type 2 cells and block their activity. Type 2 cells are consequently unable to generate allergic immune responses. This work demonstrates that the microbiota indirectly regulates type 2 immune responses by inducing type 3 cells.
These results explain how an imbalance in microbiota triggers an exaggerated type 2 immune response normally used to fight large parasites, but that also leads to allergic responses.
These findings represent an important milestone in understanding the balance between our various defense mechanisms. In terms of allergy treatment, a hitherto unexplored therapeutic approach consists therefore in stimulating type 3 cells by mimicking a microbial antigen in order to block allergy-causing type 2 cells.
These studies were funded by the French National Agency for Research, the French Medical Research Foundation, the Simone & Cino Del Duca Foundation, the European Commission and the “Integrative Biology of Emerging Infectious Diseases” Laboratory of Excellence.
Source
The microbiota regulates type 2 immunity through RORgt+ T cells, Science, July 9, 2015
Caspar Ohnmacht1*, Joo-Hong Park1*, Sascha Cording1, James B. Wing2, Koji Atarashi3,4, Yuuki Obata5, Valérie Gaboriau-Routhiau6,7,8, Rute Marques1, Sophie Dulauroy1, Maria Fedoseeva9, Meinrad Busslinger10, Nadine Cerf-Bensussan6,7, Ivo G. Boneca11,12, David Voehringer13, Koji Hase5, Kenya Honda3,14, Shimon Sakaguchi2,15, Gérard Eberl1‡
1 Institut Pasteur, Microenvironment & Immunity Unit, 75724 Paris, France
2 Laboratory of Experimental Immunology, Immunology Frontier Research Center, Osaka University, Suita 565-0871, Japan
3 RIKEN Center for Integrative Medical Sciences (IMS-RCAI), Yokohama, Kanagawa 230-0045, Japan
4 PRESTO, Japan Science and Technology Agency, Saitama 332-0012, Japan
5 The Institute of Medical Science, The University of Tokyo, Tokyo 108-8639, Japan
6 INSERM, U1163, Laboratory of Intestinal Immunity, Paris, France
7 Université Paris Descartes-Sorbonne Paris Cité and Institut Imagine, Paris, France
8 INRA Micalis UMR1319, Jouy-en-Josas, France
9 Center of Allergy and Environment (ZAUM), Technische Universität and Helmholtz Zentrum München, Munich, Germany
10 Research Institute of Molecular Pathology, Vienna Biocenter, 1030 Vienna, Austria
11 Institut Pasteur, Biology and Genetics of Bacterial Cell Wall, 75724 Paris, France
12 INSERM, Groupe Avenir, 75015 Paris, France
13 Department of Infection Biology at the Institute of Clinical Microbiology, Immunology and Hygiene, University Clinic Erlangen and Friedrich-Alexander University Erlangen-Nuremberg, 91054 Erlangen, Germany
14 CREST, Japan Science and Technology Agency, 4-1-8 Honcho Kawaguchi, Saitama 332-0012, Japan
15 Department of Experimental Pathology, Institute for Frontier Medical Sciences, Kyoto University, Kyoto 606-8507, Japan.
* Ces auteurs ont contribué équitablement à ce travail.
‡ Main author
[1] J. F. Bach, The effect of infections on susceptibility to autoimmune and allergic diseases. N Engl J Med 347, 911 (2002).