A publication published this summer looks back at the contribution of the European ZIKAlliance project, launched in 2016 following the Zika epidemic in the Pacific Islands and America. A global analysis of the competence of potential vectors was carried out, the most comprehensive study of vector competence to date using the same protocols. This study reminds us that vector-borne diseases are indeed on the list of tomorrow's pandemics.
Zika virus (ZIKV) was discovered in 1947 during a yellow fever survey conducted in the Zika Forest near Entebbe in Uganda. This virus resurfaced 70 years later with major epidemics in the Pacific Islands and in America. In 2015, the first Zika cases were diagnosed in Brazil. The infection (see Zika fact sheet) is usually asymptomatic and the symptoms are mild: moderate fever, skin rash, conjunctivitis and myalgia. More worryingly, neurological complications have been observed in this last epidemic, in particular, microcephaly in newborns and Guillain-Barré syndrome. The magnitude of the Zika outbreak prompted the WHO in 2016 to declare Zika a “public health emergency of international concern.” The European Union reacted very quickly by setting up calls for projects on Zika. The ZIKAlliance project started in 2016, bringing together 54 partners from all over the world and from various disciplines.
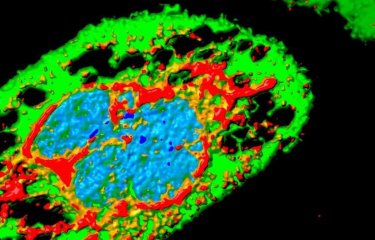
ZIKV is an arbovirus that, in most cases, requires a mosquito to ensure human-to-human transmission. In the absence of vaccines and specific treatments, the mosquito therefore remains the main target to fight Zika.
A global vector competence analysis of potential vectors (Aedes aegypti, Aedes albopictus, Aedes japonicus, Culex pipiens pipiens, Culex pipiens molestus and Culex quinquefasciatus) was performed to assess the epidemic risk associated with ZIKV. Researchers thus determined the vector competence of 50 mosquito populations from 15 localities and 12 countries (Brazil, Cambodia, Cameroon, Congo, Cuba, France, Gabon, Guadeloupe, Haiti, Reunion, Madeira, Netherlands, New Caledonia, Spain, and Switzerland). These mosquitoes were artificially infected with different ZIKV genotypes (West Africa, Asia, America). The experimental protocols were previously standardized to enable the different partners to carry out the infections under the same conditions and to allow inter-site comparisons.
This is the most comprehensive study of vector competence to date using the same protocols. The results confirm that:
- Ae. aegypti are highly competent to transmit the different Zika genotypes and more specifically, the African genotype,
- other mosquito species such as Ae. albopictus or Ae. japonicus may play a secondary role in transmission,
- and finally Culex mosquitoes are refractory to Zika infection.
Mosquitoes of the genus Aedes are invasive species whose distribution is increasing, putting many geographic regions at risk of experiencing a new Zika epidemic. After dengue fever and chikungunya, Zika reminds us that vector-borne diseases are indeed on the list of tomorrow's pandemics.
Source
Zika vector competence data reveals risks of outbreaks: the contribution of the European ZIKAlliance project, Nature Communications, August 2, 2022
Thomas Obadia1,17, Gladys Gutierrez-Bugallo2,7, Veasna Duong3, Ana I. Nuñez4, Rosilainy S. Fernandes5, Basile Kamgang6, Liza Hery7, Yann Gomard8, Sandra R. Abbo9, Davy Jiolle10, Uros Glavinic11, Myrielle Dupont-Rouzeyrol12, Célestine M. Atyame8, Nicolas Pocquet13, Sébastien Boyer14, Catherine Dauga15, Marie Vazeille15, André Yébakima16, Michael T. White17, Constantianus J. M. Koenraadt18, Patrick Mavingui8, Anubis Vega-Rua7, Eva Veronesi11, Gorben P. Pijlman9, Christophe Paupy10, Núria Busquets4, Ricardo Lourenço-de-Oliveira5, Xavier De Lamballerie19, Anna-Bella Failloux15*
1Institut Pasteur, Université Paris Cité, Bioinformatics and Biostatistics Hub, F-75015 Paris, France
2Department of Vector Control, Center for Research, Diagnostic, and Reference, Institute of Tropical Medicine Pedro Kouri, Havana, Cuba
3Institut Pasteur du Cambodge, Virology Unit, Cambodia
4IRTA, Centre de Recerca en Sanitat Animal (CReSA, IRTA-UAB), Campus de la Universitat Autònoma de Barcelona, 08193 Bellaterra, Spain
5Laboratorio de Mosquitos Transmissores de Hematozoarios, Instituto Oswaldo Cruz, Fiocruz, Rio de Janeiro, RJ, Brazil
6Centre for Research in Infectious Diseases, Department of Medical Entomology, Yaoundé, Cameroon
7Institut Pasteur of Guadeloupe, Laboratory of Vector Control research, Unit Transmission Reservoir and Pathogens Diversity, Les Abymes, Guadeloupe
8UMR PIMIT (Processus Infectieux en Milieu Insulaire Tropical), Sainte-Clotilde, La Réunion
9Laboratory of Virology, Wageningen University, Wageningen, The Netherlands
10IRD, MIVEGEC, University of Montpellier, IRD, CNRS, Montpellier, France
11National Centre for Vector Entomology, Institute of Parasitology, Vetsuisse Faculty, University of Zürich, Zürich, Switzerland
12Institut Pasteur de Nouvelle-Calédonie, URE Dengue et Arboviroses, Nouméa, Nouvelle-Calédonie
13Institut Pasteur de Nouvelle-Calédonie, URE Entomologie Médicale, Nouméa, Nouvelle-Calédonie
14Institut Pasteur du Cambodge, Medical Entomology Unit, Cambodia
15Institut Pasteur, Université Paris Cité, Arboviruses and Insect Vectors, F-75015 Paris, France
16VECCOTRA, Rivière Salée, Martinique
17Institut Pasteur, Université Paris Cité, G5 Infectious Disease Epidemiology and Analytics, F-75015 Paris, France
18Laboratory of Entomology, Wageningen University & Research, Wageningen, the Netherlands
19Unité des Virus Emergents (UVE), Aix Marseille Université, IHU Méditerranée Infection, Marseille, France
*Corresponding author. Email: anna-bella.failloux@pasteur.fr
For more information, please visit