Scientists have pinpointed the precise binding sites for the virus HKU1 in respiratory cells, providing a detailed picture of the infection mechanism used by the virus. Their findings shed light on other animal species that may host the virus and pave the way for the development of infection-blocking antibodies.
What precise mechanisms do coronaviruses use to infect us? More than four years after the infamous SARS-CoV-2 emerged in humans, many scientists are still investigating the topic. It is currently generally accepted that we can be infected with seven different coronaviruses. Some can result in lung conditions or have severe health impacts, such as SARS-CoV-2 – which causes COVID-19 – and also MERS-CoV and SARS-CoV-1. Others, like the virus HKU1, lead to milder conditions like the common cold.
Elucidating molecular structure to understand HKU1 infection
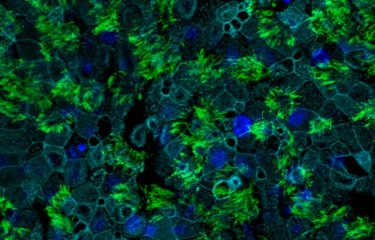
A few months ago, an important milestone was reached in HKU1 research with the identification of TMPRSS2 as a receptor molecule that enables HKU1 to bind to cells, but the precise mechanisms of infection remained unclear. In a study coordinated by scientists from the Institut Pasteur, the various steps by which HKU1 enters the cell were revealed. "We obtained a 3D atomic-scale structure of the complex formed between TMPRSS2 and the part of the HKU1 spike that binds to the receptor. This enabled us to describe the contact sites of the two proteins and the conformational changes that allow the virus to enter the target cell," explains Félix Rey, Head of the Structural Virology Unit and co-last author of the study. "We demonstrated that the cell entry mechanisms for HKU1 are different from those for other coronaviruses like SARS-CoV-2."
Three-dimensional structure of the molecular complex between the cell receptor TMPRSS2 (in pink) and the HKU1 coronavirus spike protein receptor binding domain (in blue) © Institut Pasteur/Ignacio Fernandez
Animal species carrying the virus yet to be discovered
Determining the detailed structure of the molecular complex not only improves our understanding of the infection process; it can also reveal other information. The scientists were able to identify the critical positions in the cell receptor TMPRSS2 and see whether they are also present in other animal species. They compared the sequences of TMPRSS2 equivalents in more than 200 mammal species. At two precise positions in the human cell receptor, they identified two amino acids that are essential for HKU1 infection and are not found in other animals. According to Olivier Schwartz, Head of the Virus and Immunity Unit and co-last author of the study, "macaques, pigs, mice, ferrets and hamsters, to name but a few, are therefore probably not animal reservoirs for this virus." In other words, research into the animal origin of HKU1 is still ongoing.
Antibodies to prevent infection
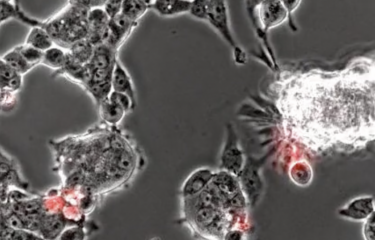
Although further research is needed to identify the origin of the virus, these latest findings also open up avenues for new therapeutic, preventive or diagnostic tools. The scientists managed to produce a mini-antibody, or nanobody (nAb): anti-TMPRSS2. The structure of the nAb/TMPRSS2 complex reveals that this antibody binds to the cell receptor at the same place as the HKU1 spike. By "taking the place" of HKU1 on the cell receptor, the nanobody prevents the virus from binding to the cell, thereby blocking infection. This is a first preventive avenue to be developed. Finally, TMPRSS2 does not just serve as a cellular anchor point for HKU1; it is also an enzyme involved in multiple physiological processes. In the long term, anti-TMPRSS2 mini-antibodies could therefore represent an effective therapeutic tool or diagnostic aid for various diseases.
This research was launched and funded by the Institut Pasteur in early 2020 in response to the COVID-19 pandemic. Several research projects related to SARS-CoV-2 and other coronaviruses are still ongoing.
Structural basis of TMPRSS2 zymogen activation and recognition by the HKU1 seasonal coronavirus, Cell, July 3, 2024
Ignacio Fernández1,8, Nell Saunders2,8, Stéphane Duquerroy1,3, William H. Bolland2, Atousa Arbabian1, Eduard Baquero4, Catherine Blanc5, Pierre Lafaye6, Ahmed Haouz7, Julian Buchrieser2, Olivier Schwartz2,*, Félix A. Rey1,9,*
1 Institut Pasteur, Université Paris Cité, CNRS UMR 3569, Structural Virology Unit, 75015, Paris, France
2 Institut Pasteur, Université Paris Cité, CNRS UMR 3569, Virus & Immunity Unit, 75015, Paris, France and Vaccine Research Institute, Créteil, France
3 Université Paris-Saclay, Faculty of Science, Orsay, France
4 Institut Pasteur, Université Paris Cité, INSERM U1222, Nanoimaging core, 75015, Paris, France
5 Institut Pasteur, Université Paris Cité, Pasteur-TheraVectys Joint Lab, Paris, France
6 Institut Pasteur, Université Paris Cité, CNRS UMR 3528, Antibody Engineering Facility-C2RT, 75015, Paris, France
7 Institut Pasteur, Université Paris Cité, CNRS UMR 3528, Crystallogenesis Facility-C2RT, 75015, Paris, France
8Equal contribution
9Lead contact