Although the biological mechanisms behind the short-term effects of COVID-19 are now known, the same is not true for long COVID. Scientists have recently demonstrated that individuals with this syndrome can present different immune responses, either weak or strong. This is a first step in improving treatment for patients with no apparent immunological traces of SARS-CoV-2 infection.
By mid-August 2023, WHO figures showed that more than 769 million people worldwide had been infected with SARS-CoV-2, leading to over 7 million deaths. The short-term signs of COVID-19 are highly variable, ranging from asymptomatic infection to severe respiratory distress. Over the longer term, patients can also experience persistent debilitating symptoms such as extreme fatigue, neurological complications, respiratory difficulties and headache. These chronic symptoms characterize a condition known as long COVID.
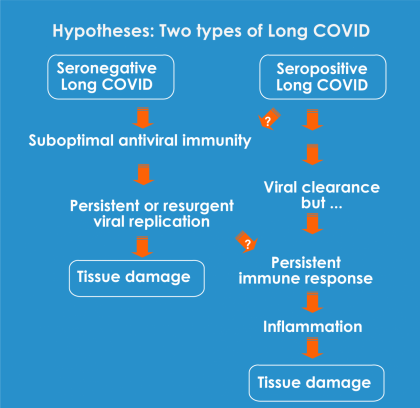
While the biological mechanisms underlying the acute phase of the disease are well documented, those that give rise to long COVID remain poorly understood. It is thought that the persistent symptoms could be caused by immune system dysfunction. Two main theories are generally put forward: an insufficient immune response that prevents the body from fully eliminating the virus, or on the contrary an excessive immune response that causes inflammatory damage.
Scientists from the Institut Pasteur, the CNRS and Inserm, in collaboration with clinicians from the Paris Public Hospital Network (AP-HP), set out to shed light on the question by analyzing antibody production and the presence of antiviral T cells in long COVID patients. The results showed that nearly a third of patients had a very weak immune response, while in the other patients the immune response was at least as strong as in individuals who had fully recovered from COVID-19. In other words, neither theory is exclusive. "Our findings suggest that there are several types of long COVID, characterized by either an insufficient antiviral response or an excessive antiviral response," explains Lisa Chakrabarti, a scientist in the Virus and Immunity Unit.
Elucidating the mechanisms behind long COVID… and facilitating access to treatment?
Although this research primarily demonstrates that there are several types of long COVID, it also paves the way for better treatment for individuals with the syndrome. As part of the study, the scientists had to use highly sensitive immunological assays to detect an immune response in "weak responder" long COVID patients for whom the standard antibody test was negative. Responses were detected in more than half of the patients who had been classified as seronegative. "If validated, these more sensitive laboratory tests could be used to help seronegative patients document their infection and facilitate their access to medical care," affirms Lisa Chakrabarti. This is a serious avenue to explore as a way of identifying long COVID patients with greater certainty. In France alone, a million people are thought to be affected by these persistent symptoms.
This study comes under the Emerging Infectious Diseases priority scientific area in the Institut Pasteur's 2019-2023 Strategic Plan
Source:
Divergent adaptive immune responses define two types of long COVID, Frontiers in Immunology, July 20, 2023
Jérôme Kervevan1, Isabelle Staropoli1, Dorsaf Slama2, Raphaël Jeger-Madiot1, Françoise Donnadieu3, Delphine Planas1, Marie-Pierre Pietri2, Wiem Loghmari-Bouchneb2, Motolete Alaba Tanah2, Rémy Robinot1, Faroudy Boufassa4, Michael White3, Dominique Salmon-Ceron2, Lisa A Chakrabarti1
1 Virus and Immunity Unit, Institut Pasteur, Université de Paris Cité, CNRS UMR3569, Paris, France.
2 Department of Infectious Diseases and Immunology, Hôtel Dieu Hospital, Assistance Publique-Hôpitaux de Paris, Université de Paris Cité, Paris, France.
3 Infectious Disease Analytics and Epidemiology G5 Unit, Institut Pasteur, Université de Paris Cité, Paris, France.
4 INSERM U1018, Center for Research in Epidemiology and Population Health (CESP), Le Kremlin-Bicêtre, France.




