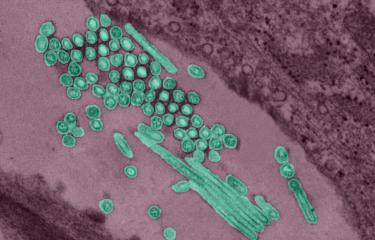
Scientists from the Institut Pasteur, Inserm and the Max Planck Institute have used high-throughput screening to identify the cellular factors involved in the replication of chikungunya virus in human cells. These findings have revealed potential therapeutic targets that could help tackle this virus.
Like all other viruses, chikungunya penetrates host cells and makes use of their cellular machinery to replicate. But little is known about the specific mechanisms used by this arbovirus (1) to enter and replicate inside cells. The teams led by Marc Lecuit* Head of the Biology of Infection Unit (Institut Pasteur/Inserm), and by Thomas Meyer from the Max Planck Institute in Berlin therefore set themselves the task of identifying the cellular genes involved in the replication of the virus by inhibiting them systematically, one by one, to examine the effect of their inhibition on viral replication.
They used the technique of high-throughput screening: human cells were cultured in thousands of wells in the screening platform together with interfering RNAs (2) – each one inhibiting a given gene – and were infected by chikungunya virus. "We used a virus that induces fluorescence in the cell it infects. The intensity of the fluorescence indicates the extent of the infection," explained Marc Lecuit. "If the fluorescence decreases, it means that the gene which has been blocked is required for infection and that it plays a proviral role. But if the fluorescence increases, it shows that the inhibited gene has an antiviral role." A total of 156 proviral genes – involved for example in transporting the virus – and 41 antiviral genes were identified.
The scientists used these findings to pinpoint the cellular factors necessary for the replication of chikungunya virus and to identify signaling pathways that can be targeted for therapeutic purposes. Various molecules with the potential to inhibit the gene products or signaling pathways identified by the scientists were tested in vitro in cell models and in vivo in mouse models. They found that some drugs, on their own or in combination, showed antiviral efficacy against both chikungunya virus and also other viruses, including influenza and herpes, which use similar cellular pathways to replicate.
"The development of effective anti-infective treatments relies on a thorough understanding of the biological mechanisms involved in infection. The understanding of the biological mechanisms underpinning the replication of the HIV or hepatitis C virus has enabled the development of extremely effective treatments against these viruses," explains Marc Lecuit. "When it comes to emerging viruses such as chikungunya, which we naturally know much less about, it can be useful to focus on the cellular genes involved in infection, against which inhibitors exist, rather than trying to target the virus directly, so that we can try to identify new therapeutic targets as quickly as possible."
(1) a virus transmitted by bites from arthropods, particularly mosquitoes.
(2) Paris Descartes – Sorbonne Paris Cité University, Necker-Enfants Malades Hospital, AP-HP.
(3) small RNAs that can specifically impair a messenger RNA sequence and prevent expression of the corresponding gene.
Source
A human genome-wide loss-of-function screen identifies effective chikungunya antiviral drugs, Nature Communications, May 12, 2016.
Alexander Karlas (1,2)*, Stefano Berre (3,4)*, Thérèse Couderc (3,4), Margus Varjak (5), Peter Braun (1,2), Michael Meyer (2), Nicolas Gangneux (3,4), Liis Karo-Astover (5), Friderike Weege (1), Martin Raftery (6), Günther Schönrich (6), Uwe Klemm (7), Anne Wurzlbauer (8), Franz Bracher (8), Andres Merits (5), Thomas F. Meyer (1,2)** & Marc Lecuit (3,4,9)**
1 Max Planck Institute for Infection Biology, Department of Molecular Biology, Charité platz 1, 10117 Berlin, Germany.
2 Steinbeis Innovation gGmbH, Center for Systems Biomedicine, Haydnallee 21, 14612 Falkensee, Germany.
3 Institut Pasteur, Biology of Infection Unit, 28 rue du Dr. Roux, 75015 Paris, France.
4 Inserm U1117, 28 rue du Dr. Roux, 75015 Paris, France.
5 Institute of Technology, University of Tartu, Nooruse 1, 50411 Tartu, Estonia.
6 Institute of Virology, Charite ́ University Medicine, Charité platz 1, 10117 Berlin, Germany.
7 Max Planck Institute for Infection Biology, Core Facility Experimental Animals, Charité platz 1, 10117 Berlin, Germany.
8 Ludwig-Maximilians-University, Department of Pharmacy-Center for Drug Research, Butenandtstrasse 5-13, 81377 Munich, Germany.
9 Paris Descartes University, Sorbonne Paris Cité, Division of Infectious Diseases and Tropical Medicine, Necker-Enfants Malades University Hospital, Institut Imagine, 149, rue de Sèvres 75743 Paris, France.
* These authors contributed equally to this work. ** These authors jointly supervised this work.
Mis à jour le 12/05/2016