Dominant optic atrophy (DOA) is one of the most common forms of mitochondrial disease. It can be caused by genetic mutations in OPA1 resulting in mitochondrial dysfunction. Researchers from Institut Pasteur and CNRS found ways to study and modulate the effect of genetic mutations in OPA1.
Genetic mutations in the gene Optic Atrophy 1 (OPA1) cause a disease named Dominant optic atrophy (DOA). Most patients develop isolated optic atrophy, which is a deterioration of the optic nerve, yet about 20% of patients develop more severe neurological disease (DOA+) that cannot be fully explained by the location or nature of the disease-causing mutation in OPA1.
High-throughput screening helps identify genes that could suppress mitochondrial fragmentation
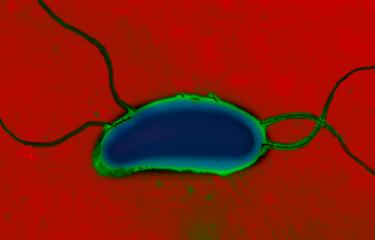
“We developed a mitochondrial imaging and analysis pipeline that allowed us to perform high-throughput phenotypic screening of primary fibroblast from patients suffering from DOA+.” Explains Timothy Wai, CNRS researcher and head of the Mitochondrial Biology group at Institut Pasteur. One of the effects of the genetic mutation is mitochondrial fragmentation, a phenomenon in which the mitochondria splits into small vesicles. His team screened 1531 genes coding for the mitochondrial proteome (the proteins that constitutes the mitochondria) and found 91 genetic modifiers that could suppress mitochondrial fragmentation in patient-derived fibroblasts.
This discovery demonstrates for the first time that the action of other mitochondrial proteome genes can influence the defects caused by OPA1 deficiency and illustrates the genetic complexity of this rare disease. Moreover, the screening approach they developed could be used for a more personalized characterization of DOA applied directly in the cells of patients that suffer from this incurable disease.
Source:
High-throughput screening identifies suppressors of mitochondrial fragmentation in OPA1 fibroblasts. EMBO Molecular Medicine, 20 may2021
Emma Cretin1,2, Priscilla Lopes1, Élodie Vimont1, Takashi Tatsuta3, Thomas Langer3,4, Anastasia Gazi5, Martin Sachse5, Patrick Yu-Wai-Man6-9, Pascal Reynier10,11, Timothy Wai1,2
1Mitochondrial Biology Group, Institut Pasteur, CNRS UMR 3691, Paris, France 2Université de Paris, Paris, France 3Max-Planck-Institute for Biology of Ageing, Cologne, Germany 4Cologne Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD), University of Cologne, Cologne, Germany 5UTechS Ultrastructural Bio Imaging, Institut Pasteur, Paris, France 6Cambridge Centre for Brain Repair and MRC Mitochondrial Biology Unit, Department of Clinical Neurosciences, University of Cambridge, Cambridge, UK 7Cambridge Eye Unit, Addenbrooke's Hospital, Cambridge University Hospitals, Cambridge, UK 8Moorfields Eye Hospital, London, UK 9UCL Institute of Ophthalmology, University College London, London, UK 10Laboratoire de Biochimie et biologie moléculaire, Centre Hospitalier Universitaire, Angers, France 11Unité Mixte de Recherche MITOVASC, CNRS 6015, INSERM U1083, Université d'Angers, Angers, France