A new technique could provide vital information about a community’s immunity to infectious diseases including malaria and Covid-19.
The diagnostic test analyses a blood sample to reveal immune markers that indicate whether – and when – a person was exposed to an infection. It was developed to track malaria infections in communities, to assist in the elimination of deadly ‘relapsing’ malaria, but is now being adapted to track immunity to Covid-19 in more detail than existing tests.
This new diagnostic approach, published in Nature Medicine, has the potential to enhance infectious diseases surveillance – particularly in lower income countries where it can enable health authorities to track the spread of a disease in a community and target resources where they are most needed. The research was led by researchers from Institut Pasteur, France; the Walter and Eliza Hall Institute, Australia; and Ehime University, Japan.
At a glance
- An international team has developed a new approach to detecting a person’s immunity to an infectious disease – providing valuable details about whether and when a person was exposed to the infection.
- The test was developed for detecting recent exposure to malaria, but the research team are now working to adapt it to detect previous exposure to the coronavirus that causes Covid-19.
- By providing a detailed picture of when an infection spread in a community, the test offers new opportunities for improving infection control and elimination strategies – particularly in lower income countries.
Detecting past infections
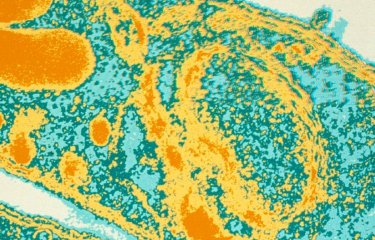
Exposure to viruses, parasites or bacteria triggers immune responses that lead to antibodies circulating in the blood. These antibodies can remain for years, but over time the amount of different types of antibodies changes.
The new diagnostic technique allows researchers to look in detail at the amounts of different antibodies in the blood, to pinpoint whether – and importantly when – a person has been exposed to a particular infection, said Professor Ivo Mueller, who led the research and has joint appointments at the Walter and Eliza Hall Institute and Institut Pasteur.
“Many tests for immunity give a simple ‘yes or no’ answer to whether someone has antibodies to the infectious agent,” he said. “In contrast, our test – which was initially developed to look at malaria infections – can pinpoint how long ago a person was exposed to an infection.
“This information is extremely valuable for tracking the spread of an infection in a population. Particularly in lower income countries it may not be possible to monitor the actual spread of the infection, but it is very helpful to look retrospectively at whether the infection has been spreading – and to monitor the effectiveness of infection control programs, and respond to disease resurgence,” he said.
The team established this research to understand the spread of relapsing ‘vivax’ malaria. The parasite causing this form of malaria – the most widespread malaria parasite in the world – can be carried in a dormant state by people and later reawaken to continue to disease spread, causing significant challenges for malaria control.
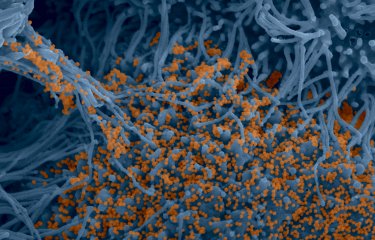
Professor Mueller said that his team in Paris and Melbourne were now applying the systems they have established for malaria to detect immunity to the coronavirus that causes Covid-19.
“We have already started to study the blood of people who have had Covid-19 infections to document the types of antibodies they carry. In the next six months we hope to have discovered how these antibodies change over time, meaning we can use this information to explore immunity in wider groups in the community.
“This is not a tool for diagnosing individual people, but rather for monitoring Covid-19 disease spread in populations. In many countries in Africa and Asia it is possible that Covid-19 will be spreading undetected in some regions for the coming year – especially as governments try to loosen shutdown restrictions. This test could be invaluable for informing these decisions.”
A research project, funded by the Institut Pasteur, is currently launched in West Africa, using this new diagnostic approach for serological surveillance of SARS-CoV-2 and seasonal coronaviruses. This project involves four members of the Institut Pasteur International Network: Institut Pasteur à Paris, Institut Pasteur de Dakar, Pasteur Center in Cameroon et Institut Pasteur de Côte d'Ivoire.
Eliminating malaria
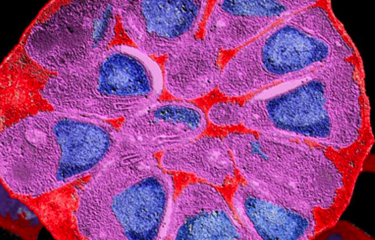
Institut Pasteur researcher and joint lead author Dr Michael White said the malaria blood test had been validated using samples contributed by people living in malaria-endemic regions of Brazil, Thailand and the Solomon Islands.
“Our investigations confirmed that the test could detect people who had been infected with P. vivax in the preceding nine months – and who would thus be at risk of recurring malaria infections,” Dr White said.
“This information will enable better surveillance and deployment of resources to areas where malaria remains, and targeted treatment of infected individuals. This could be a huge improvement in how vivax malaria is controlled and eventually eliminated.”
“Our team are now working with Axxin, an Australian biotech company, to develop a diagnostic test for malaria that can be deployed in the field, based on the immune markers our laboratory testing identified,” Professor Mueller said. “We plan to continue clinical trials investigating how our test can guide malaria elimination efforts, and having a rapid field test will be an important aspect of this.”
The research underpinning the new test was led by Professor Mueller and Dr White, with Dr Rhea Longley from the Walter and Eliza Hall Institute in Melbourne and Professor Takafumi Tsuboi from Ehime University in Japan.
Funding for this research was provided by the Walter and Eliza Hall Institute Innovation Fund, Global Health Innovative Technology Fund, The Foundation for Innovative New Diagnostics, United States National Institute of Allergy and Infectious Diseases, TransEPI consortium (supported by the Bill & Melinda Gates Foundation), National Research Council of Thailand, Japan Society for the Promotion of Science, Howard Hughes Medical Institute, Wellcome Trust (UK), Brazilian National Council for Scientific and Technological Development, United Kingdom Government, Australian National Health and Medical Research Council and Victorian Government.
Sources
Development and validation of serological markers for detecting recent Plasmodium vivax infection, Nature Medicine, May 11, 2020.
Rhea Longley1,2,3,21, Michael White4,21, Eizo Takashima5, Jessica Brewster1, Masayuki Morita5, Matthias Harbers6,7, Thomas Obadia4,8, Leanne Robinson1,2,9, Fumie Matsuura6, Zoe Liu1,2, Connie Li-Wai-Suen1,2, Wai-Hong Tham2,10, Julie Healer2,10, Christele Huon11, Chetan Chitnis11, Wang Nguitragool12, Wuelton Monteiro13,14, Carla Proietti15,16, Denise Doolan15,16, Andre Siqueira17, Xavier Ding18, Iveth Gonzalez18, James Kazura19, Marcus Lacerda13,20, Jetsumon Sattabongkot3, Takafumi Tsuboi5, Ivo Mueller1,2,4
1. Population Health and Immunity Division, Walter and Eliza Hall Institute of Medical Research, Melbourne, Victoria, Australia.
2. Department of Medical Biology, University of Melbourne, Melbourne, Victoria, Australia.
3. Mahidol Vivax Research Unit, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand.
4. Unité Malaria: Parasites et Hôtes, Département Parasites et Insectes Vecteurs, Institut Pasteur, Paris, France.
5. Division of Malaria Research, Proteo-Science Center, Ehime University, Matsuyama, Japan.
6. CellFree Sciences Co., Ltd., Yokohama, Japan.
7. RIKEN Center for Integrated Medical Sciences (IMS), Yokohama, Japan.
8. Hub de Bioinformatique et Biostatistique, Département Biologie Computationnelle, Institut Pasteur, USR 3756 CNRS, Paris, France.
9. Burnet Institute, Melbourne, Victoria, Australia.
10. Infection and Immunity Division, Walter and Eliza Hall Institute of Medical Research, Melbourne, Victoria, Australia.
11. Malaria Parasite Biology and Vaccines, Department of Parasites & Insect Vectors, Institut Pasteur, Paris, France.
12. Department of Molecular Tropical Medicine and Genetics, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand.
13. Fundacão de Medicina Tropical Dr. Heitor Vieira Dourado, Manaus, Brazil.
14. Universidade do Estado do Amazonas, Manaus, Brazil.
15. Centre for Molecular Therapeutics, Australian Institute of Tropical Health and Medicine, James Cook University, Cairns, Queensland, Australia.
16. QIMR Berghofer Medical Research Institute, Brisbane, Queensland, Australia.
17. Instituto Nacional de Infectologia Evandro Chagas–Fiocruz, Rio de Janeiro, Brazil.
18. Foundation for Innovative New Diagnostics, Geneva, Switzerland.
19. Center for Global Health and Diseases, Case Western Reserve University, Cleveland, OH, USA.
20. Instituto Leônidas & Maria Deane (Fiocruz), Manaus, Brazil.
21. These authors contributed equally: Rhea J. Longley, Michael T. White.
Serological signatures of SARS-CoV-2 infection: Implications for antibody-based diagnostics, HAL Pasteur, May 11, 2020.
Jason Rosado1, Charlotte Cockram2, Sarah Merkling3, Caroline Demeret4, Annalisa Meola5, Solen Kerneis6,7, Benjamin Terrier8,9, Samira Fafi-Kremer10, Jérome Sèze11, Marija Backovic5, Ivo Mueller1,12, Michael White1
1. Malaria: Parasites and Hosts Unit, Department of Parasites and Insect Vectors, Institut Pasteur, Paris, France
2. Spatial Regulation of Genomes Unit, Department of Genomes and Genetics, Institut Pasteur, Paris, France
3. Insect-Virus Interactions Unit, Department of Virology, UMR 2000, CNRS, Institut Pasteur, Paris, France
4. Molecular Genetics of RNA Viruses Unit, Department of Virology, Institut Pasteur, Paris, France
5. Structural Virology Unit, Department of Virology and CNRS UMR 3569, Institut Pasteur, Paris, France
6. Equipe Mobile d’Infectiologie, APHP Centre-Université de Paris, Paris, France
7. Epidemiology and Modelling of Bacterial Escape to Antimicrobials Unit, Department of Global Health, Institut Pasteur, Paris, France
8. Department of Internal Medicine, National Referral Center for Rare Systemic Autoimmune Diseases, Assistance Publique Hôpitaux de Paris-Centre (APHP-CUP), Université de Paris, Paris, France
9. PARCC, INSERM U970, Paris, France
10. CHU de Strasbourg, Laboratoire de Virologie, F-67091 Strasbourg, France
11. Université de Strasbourg, INSERM, IRM UMR_S 1109, Strasbourg, France
12. Centre d'Investigation Clinique -INSERM CIC-1434, Strasbourg, France
13. Division of Population Health and Immunity, The Walter and Eliza Hall Institute, Melbourne, Australia