The Institut Pasteur, in collaboration with Johnson & Johnson Innovative Medicine Research & Development, uncovers the interactions between a molecule (the cytokine interleukine-23 (IL-23)) produced by the immune system and so-called mucosal-associated invariant T (MAIT) cells, which are involved early in the immune response to fight pathogens.
Chronic inflammatory diseases are clinically heterogeneous, but they share common inflammatory pathways and are caused by aberrations in the immune response.
Previously studied in mouse models of autoimmune diseases and through genome-wide association studies (GWAS), IL-23 is increasingly recognized as an essential player in various chronic inflammatory conditions, notably Crohn’s disease, spondylarthritis and psoriasis. Data also suggest that IL-23 plays a role in the response against certain infectious agents.
A study led by Lars Rogge, head of the Immunoregulation Unit at the Institut Pasteur, in collaboration with Johnson & Johnson Innovative Medicine Research & Development (J&J IM R&D) and other teams at the Institut Pasteur (including the biomarker platform and the Bioinformatics and Biostatistics Hub, and the team directed by Laura Cantini), provides new insights into the interactions between this key molecule of the immune system, IL-23, and MAIT cells.
Which cells in our body respond to IL-23?
IL-23 is a “messenger” (a cytokine) produced by our body to alert and activate immune cells. Scientists already knew about its involvement in the development of several inflammatory diseases, but the exact targets of IL-23 within the immune system and the precise mechanisms of its action remain unclear.
By conducting in-depth cellular and molecular analyses on human patient samples, researchers at the Institut Pasteur and in J&J IM R&D focused on a type of T lymphocyte called MAIT (for “mucosal-associated invariant T”). These cells act as “sentinels”: they are found especially in mucosal tissues, where they rapidly detect the presence of certain microbial metabolites. In other words, MAIT cells intervene early in the immune response to combat pathogens.
The team observed that most MAIT cells express IL-23 receptors (called IL-23R). This means these cells are particularly sensitive to the “signal” transmitted by IL-23.
The Plasticity of MAIT Cells
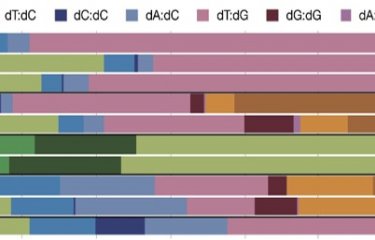
When stimulated with IL-23 (or related cytokines such as IL-12), MAIT cells change their behavior: they produce different molecules, specialize in various immune tasks, and can adapt very precisely to the body’s needs. This “plasticity” is crucial, as it partly explains how our immune system can respond to a wide range of threats, whether they are bacteria, fungi, or even cells that might be dangerous to the individual (e.g. autoimmunity or tumor development).
New perspectives in therapeutic approaches
By demonstrating that IL-23 has a strong effect on MAIT cells, this work paves the way for future research aimed at improving existing treatments to inhibit IL-23, in particular to block this signal in diseases where IL-23 plays a deleterious role (e.g., Crohn’s disease, psoriasis, or psoriatic arthritis). The findings also highlight the potential to explore how to optimize or “reactivate” IL-23 to boost immune defenses.
Finally, the “plasticity” of MAIT cells, which can change function depending on the stimuli, could be leveraged to develop new immunotherapeutic treatments that precisely target the right MAIT cell subpopulation.
Ce travail résulte d'une collaboration étroite et initiée de longue date en matière de R&D entre le laboratoire de Lars Rogge et J&J IM R&D, et implique également des cliniciens de l'AP-HP.
The article can be accessed at: https://doi.org/10.1016/j.isci.2025.111898