Preventive vaccination is a powerful tool in controlling viral outbreaks. It is important that any side effects associated with the use of vaccines are as mild as possible. Scientists from the Institut Pasteur set out to understand the reasons behind the rare neurological side effects that occasionally occur with use of the yellow fever vaccine. They studied a vaccine strain known as FNV, which stopped being used in the 1980s because it caused a high number of neurological side effects. The conclusions drawn from the analysis of this former vaccine can yield valuable lessons for current vaccines.
The current yellow fever vaccine is a highly effective live attenuated vaccine. It is considered to be one of the most well tolerated of all vaccines produced from live attenuated viruses. The vaccine, known as Stamaril, is widely used to tackle outbreaks in South America and on the African continent, which still cause more than 70,000 deaths each year.
In very rare cases, neurological side effects may be observed (0.000012–0.00002% of vaccinated patients). But given the considerable benefits of the vaccine, the recommendations for risk areas remain the same: under international regulations, yellow fever vaccination is required before traveling to an endemic area (a vaccination certificate is needed to enter endemic countries). A single injection confers long-term protection (see the Institut Pasteur fact sheet).
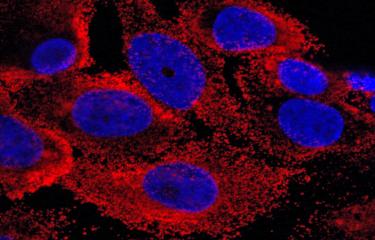
The aim of the research carried out by the Viral Neuro-Immunology and Virus Sensing and Signaling Units at the Institut Pasteur, with their academic partners (Sorbonne University and the Institute for Integrative Biology of the Cell) and their industrial partner (Sanofi Pasteur), was to shed light on the viral determinants behind these side effects – in particular how vaccine particles, together with the viruses transported by the bloodstream, manage to access the brain, which is normally protected from unwanted substances by the blood-brain barrier.
The neuroinvasiveness of variants is a cooperative phenomenon
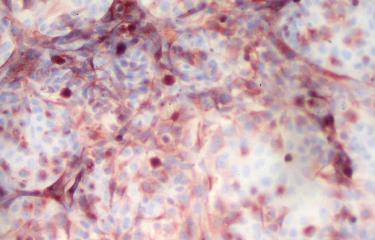
The scientists used a model of the blood-brain barrier and a vaccine strain known as FNV (French neurotropic vaccine), which was discontinued in the 1980s because it led to a higher frequency (0.3%) of encephalitis. The scientists confirmed that, compared with the Stamaril vaccine strain, the FNV strain was more heterogeneous and crossed the blood-brain barrier model more often. "In the vaccine batch, we identified several FNV variants that were capable of effectively crossing the blood-brain barrier model," explains Nolwenn Jouvenet, Head of the Virus Sensing and Signaling Unit. "But against all expectations, once they had been isolated and studied individually, none of the variants were more neuroinvasive than the original strain." The variants only became neuroinvasive once they had been mixed together, which suggests that the ability of the FNV strain to cross the blood-brain barrier model is a cooperative phenomenon. It therefore appears that the more variants a vaccine contains, the more easily it will be able to access the brain.
The conclusion of this study suggests that the safety of a live yellow fever vaccine depends on its low genomic diversity. This parameter is an important point to take into account in the production of live virus vaccines.
Source :
Genomic diversity contributes to the neuroinvasiveness of the Yellow fever French neurotropic vaccine, nature partner journals Vaccines, 26 April 2021
Florian Bakoa1,2,3,,6, Christophe Préhaud1,6, Guillaume Beauclair 4,5, Maxime Chazal4, Nathalie Mantel2, Monique Lafon1 and Nolwenn Jouvenet 4
1Unité de Neuroimmunologie Virale, Institut Pasteur, Paris, France.
2Research and External Innovation Department, Sanofi Pasteur, Marcy L’Etoile, Lyon, France.
3Sorbonne Université, Collège doctoral, Paris, France.
4Unité de Signalisation Antivirale, CNRS UMR 3569, Institut Pasteur, Paris, France.
5Institut de Biologie Intégrative de la Cellule, UMR9198, Équipe Autophagie et Immunité Antivirale, Faculté de Pharmacie, Châtenay-Malabry, Paris, France.
6These authors contributed equally
This study is part of the Vaccinology and Immunotherapy Initiative of the Institut Pasteur's strategic plan for 2019-2023.