In recent years, progress in research on hearing mechanisms and the factors responsible for hearing disorders has raised hopes for future preventive and curative therapies. Currently the only solutions for hearing loss are external hearing aids and cochlear implants. The issue is becoming increasingly urgent given the number of people affected by hearing loss, the most common sensory disorder in humans. The Hearing Institute, an Institut Pasteur research center inaugurated a year ago, has the ambition to understand auditory perception and is a great hope for people with hearing loss.
In France, 65% of over 65s affected
According to the World Health Organization (WHO), 5% of the global population is affected by hearing loss. The figures are staggering: 466 million people worldwide currently have disabling hearing loss, including 34 million children, and by 2050 more than 900 million people will be affected – that's one in ten! In France, 6 million people are affected by hearing loss – a thousand babies are born deaf every year, and the percentage of people with hearing loss in the population increases with age: 6% between the ages of 15 and 24, 9% between 25 and 34, 18% between 35 and 44, and more than 65% over the age of 65 (1 person in 3 between the ages of 65 and 75, and 1 in 2 over the age of 80).
Overcoming communication barriers
Hearing loss can therefore occur at any age and at varying levels of severity, causing anything from mild difficulties to major communication problems. In newborns, hearing loss is particularly problematic since hearing is vital for acquiring speech, which plays such a key role in communication. The flow of auditory information to the areas of the brain that deal with language is essential in the first 6 years of life and especially between the ages of 0 and 3. Profound hearing loss that is not corrected by a hearing aid will prevent the spontaneous acquisition of oral language. Children with mild hearing loss may acquire language, but their hearing impairment will have an impact on learning at school, cognitive development and social adjustment. Regardless of the age at which it occurs, hearing loss considerably complicates social interactions – having difficulties hearing or being unable to hear others can lead to social isolation, resulting in psychological distress which can culminate in depression in some people. Hearing loss is often associated with cognitive decline, especially in elderly people (memory loss, concentration problems, etc.). It was recently discovered that hearing loss is the main modifiable risk factor for the onset of neurodegenerative diseases (see below).

The Cognition and Auditory Communication team led by Luc Arnal and Diane Lazard at the Hearing Institute is attempting to understand how the brain processes the complex signals – verbal, non-verbal or musical – in audio communication and adapts its behavioral responses accordingly. This adaptation can have a negative effect, as Diane Lazard explains. The scientist has identified factors that could explain the failure of implants (in 5 to 10% of cases) in adults who have developed profound hearing loss*: "Subconsciously, the patients compensate for their hearing impediment either by lip reading or by becoming "super-readers," who are capable of handling written words better than people without hearing loss. In these patients, implants yield poor results. Lip reading maintains a central phonological organization very similar to that of normal-hearing people (using the left hemisphere of the brain), while the replacement of orality by written exchanges in "super-readers" uses different circuits, in the "right brain": they develop "supra-natural" visual capabilities but lose auditory communication abilities, which represents a handicap for the use of implants." Other surprising studies aim to help us understand why some sounds are perceived as being unpleasant, particularly by those with anxiety. "We have shown that listening to "rough sounds," characterized by certain frequencies not generally used except to signal danger, targets not only the auditory cortex but also archaic brain networks linked with reflex reactions, which affect the listener's state of stress and alertness," explains Luc Arnal. These networks seem to be affected in Alzheimer's patients. In mouse models exposed to these harsh sounds for one hour a day, the protein markers for the disease decreased. Could such sounds be used for therapeutic or diagnostic purposes? "We are launching a study in patients aged around 60 with the first signs of Alzheimer's (presymptomatic patients) to look for any disturbances when they listen to these sounds," says the scientist, who is also interested in music: "Music stimulates predictive mechanisms in the processing of sound; if exposed to a repeated rhythm, for example, the brain will wait and synchronize itself with this rhythm. Hallucinations in schizophrenic patients could be caused by an excess of brain predictions." This research, using psychoacoustic, neuroimaging and neurocomputational modeling methods, is being conducted on volunteers in collaboration with the CERIAH (see p. 3).
* Study carried out at the Institut Vernes in Paris, where Diane Lazard is an ENT surgeon, in collaboration with the University of Geneva (published in 2017).
Three in four cases of hearing loss in infants caused by genetic factors
How does hearing loss occur? There are many causes: at birth ("congenital" hearing loss) it is caused by genetic factors in three quarters of cases, with the other quarter often being associated with an infection in the mother (e.g. cytomegalovirus) or the use of "ototoxic" drugs during pregnancy. During childhood, it can be caused by ear infections or measles. The major factors responsible for hearing loss over a person's lifetime are exposure to excessive noise and aging (see inset on noise). In these cases too, genetic factors play a part, with some individuals being more susceptible to deterioration than others. In the field of genetics there have been impressive advances in research in recent years, leading to considerable progress in our understanding of how the ear works, and in medical terms to better treatment for children with deafness or hearing loss.
According to WHO, more than a billion young people (aged 12 to 35) are currently at risk of hearing loss because of exposure to recreational noise – at entertainment venues such as concerts and sporting events, and especially from listening to loud music for long periods via personal audio devices. Noise is also on the rise in urban areas, which are currently home to 56% of the world's population (68% by 2050). "Over-exposure to noise is the main threat to the auditory system, at all ages and worldwide," explains Aziz El-Amraoui, Head of the Progressive Sensory Disorders, Pathophysiology and Therapy Unit at the Hearing Institute. "We are currently elucidating the mechanisms involved in the emergence, progression and severity of hearing loss, and especially the impact of exposure to noise." The hope today is "to identify therapeutic avenues to prevent, slow, curb or correct hearing decline," continues Aziz El-Amraoui.

Since 2015, the laboratory run by Christine Petit has been conducting research into genetic factors that predispose humans to hearing loss caused by over-exposure to noise. In a first study,* she and her colleagues revealed a genetic condition responsible for early-onset hearing loss in humans and showed that this genetic defect caused hearing loss even on exposure to soft sounds, the equivalent to a minute in a nightclub. These sounds were enough to damage the auditory sensory cells and their neurons, which ultimately died in the event of prolonged or repeated exposure. With her colleagues in the Fundamental Mechanisms of Hearing and Precision Medicine laboratory and with Paul Avan, she is currently developing a large-scale study conducted jointly with IRBA, designed to identify not only genes underpinning vulnerability to noise but also biomarkers that point to underlying conditions. The results of the study will be used to develop therapies and to optimize the chances of success of therapeutic trials.
* In collaboration with the Laboratory of Sensory Biophysics, led by Professor Paul Avan at the University of Auvergne.
.
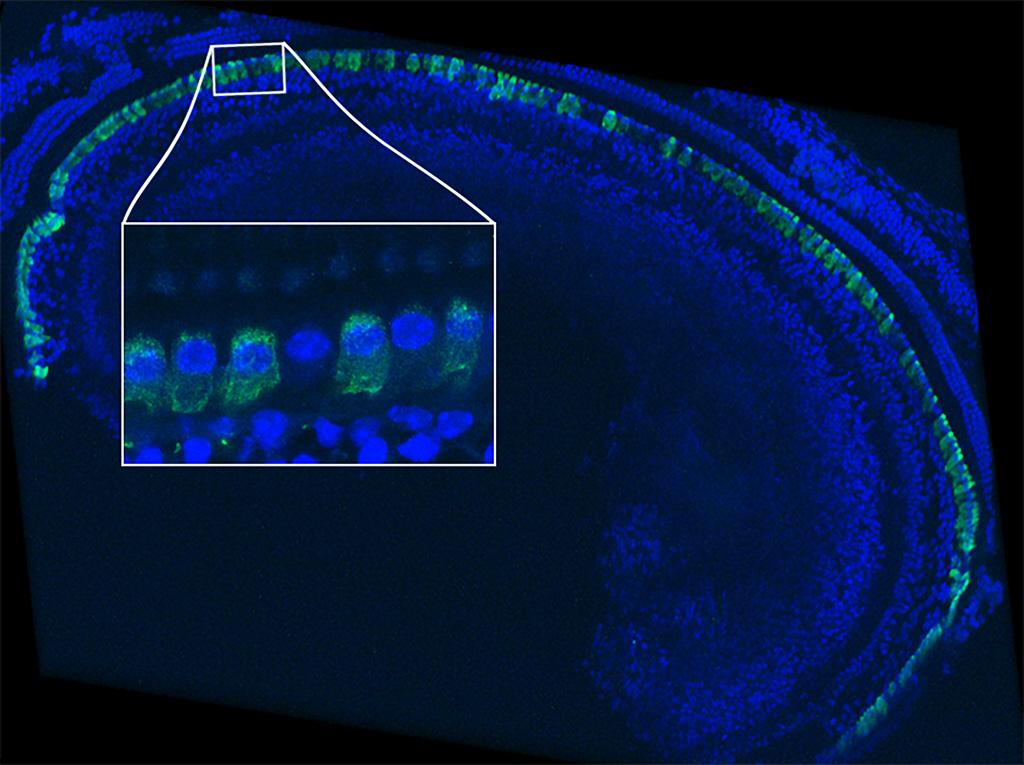
Detecting neonatal hearing loss as early as possible
In the 1990s, the causes of hearing impairments in children born deaf were not known. A team of Institut Pasteur scientists (see Interview) localized the first genes associated with hearing loss. By studying several individuals in families particularly affected by hearing loss, around 20 genes were identified, including connexin 26, discovered in 1997, which alone is responsible for half of all cases of hereditary hearing loss. Some 130 genes responsible for "monogenic" congenital hearing loss (caused by a defect in a single gene) are now known. This progress in research has led to genetic diagnosis of hereditary hearing loss, now performed routinely in several countries. Early diagnosis is vital – the earlier a child's hearing impairment can be corrected, for example with a cochlear implant, the less impact it will have on his/her linguistic and learning capabilities. Knowing which gene is responsible can also inform the decision about the potential benefits of a hearing aid, since cochlear implants are unfortunately not suitable for some genetic impairments.


The opening of an institute for hearing reflects the ambition to understand auditory perception and represents a beacon of hope for those with hearing loss.
You lead the Hearing Institute, an Institut Pasteur research center inaugurated on February 28. What is the aim of the center?
The Hearing Institute was set up in response to the need to advance our understanding of auditory perception and the ambition to develop this field of medicine. These two aims are part of a broader research dynamic that places particular emphasis on developing the interface between them. Achieving progress in both areas will require them to be firmly rooted in high-level expertise and research. The idea is to develop an integrative approach to the auditory system to help elucidate the workings of auditory perception, the nature of the acoustic signals on which it is based, the ways in which information is extracted from these signals, how perception is shaped by past experience and emotion, how it contributes to a unified multi-modal perception, how speech and music trigger specific appropriate responses, which neural networks are involved in the representation of sounds, how their plasticity is controlled, etc. We are also aiming to develop translational research which draws on scientific advances made primarily in animals and individuals without hearing loss (regarding cognitive aspects), so that they can be transposed into advances in diagnostics and therapeutics: designing new tools to explore hearing and innovative methods for diagnosing hearing impairments that will improve indications and the adjustment of hearing aids, developing effective treatments for the cochlea and cochlear neurons – initially based on gene and pharmacological therapy –, improving surgical techniques for administering therapeutics through robotic approaches, moving beyond empirical approaches to the auditory rehabilitation needed after restoring hearing and instead adopting approaches based on scientific knowledge, and paving the way for long-term therapeutic developments aimed at transmitting sensory information directly to targeted neural populations in the brain. The Hearing Institute is associated with Inserm and some of its scientists are at the CNRS. It has around ten research teams and a Center for Research and Innovation in Human Audiology (CERIAH), which represents the cornerstone of medical progress. One of the innovative aspects of the institute is its interdisciplinary nature: it brings together scientists from a variety of scientific disciplines (biophysics, audiology, neurophysiology, computational neuroscience, genetics and genomics, cell biology, etc.) and medical fields (ENT physicians, hearing aid specialists, etc.). Its aim is also to transfer knowledge and meet the need for information among those with hearing loss.
What has been the reaction to the institute?
The opening of a dedicated institute for hearing was a major event that was welcomed with great enthusiasm by the international scientific community! The institute opened at a time of growing global realization of the extent to which hearing loss is a public health challenge and increasing awareness of the real danger of sound pollution for hearing. We are currently also seeing a real commitment to research into innovative therapies supported by the development of a new industry sector.
As the leader of a pioneering team searching for genes associated with hearing loss and investigating the auditory system, can you sum up the current state of research?
We ushered in the possibility of genetic approaches to hearing by identifying several genes responsible for hearing loss in humans, and this has contributed to a molecular-level understanding of the development and workings of the auditory system. It was the convergence of progress in biophysics, physiology and genetics – all scientific approaches represented at the Hearing Institute – and the consolidation of results in all these areas that led to such a major step forward in our knowledge of the auditory system. This enabled us to reveal key molecular complexes involved in the processing of sound and to elucidate their properties. As a corollary to this approach, we were also able to unravel the defective mechanisms in each form of early-onset hearing loss. As soon as the first genes associated with hearing loss were identified, molecular diagnosis of early-onset hearing loss began to be developed.
The Institut Pasteur has focused a great deal of effort in this area, especially in developing countries. This knowledge, which of course is still in its early stages, demonstrates that the search for effective therapies for hearing loss is realistic. The development of gene therapy to treat genetic disorders was logically the first avenue to be explored, but the pharmacological approach is also gaining ground; cochlear cell regeneration is particularly promising. The aim today is to understand the mechanisms behind presbycusis so that it can be treated. This is the reason for the research efforts in which several teams and of course the CERIAH are involved. To initiate a major, long-term change in our field, we are convinced of the need for innovative teaching. We are particularly committed in this area and are working to develop practical and theoretical teaching aimed at scientists, physicians, engineers, hearing aid specialists and speech therapists.

"Hearing molecules"
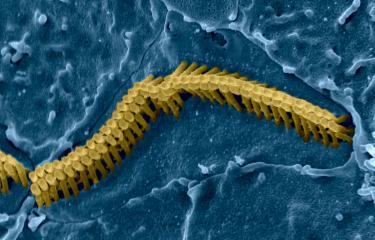
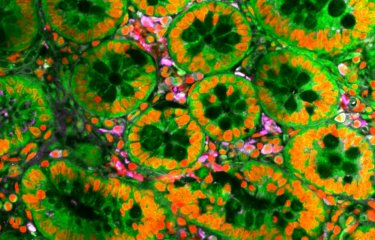
Studying the proteins encoded by genes associated with hearing loss has also shed light on how our hearing system works at the molecular level, especially the mechanisms underpinning the auditory sensory organ, the cochlea, in the inner ear (read How does hearing work?). The cochlea is a difficult organ to study, since it is embedded in the temporal bone and is composed of barely 15,000 auditory sensory cells (by way of comparison, the sensory organ for vision, the retina, which is directly observable, has more than 100 million photoreceptors). Research is under way to produce "miniature cochleas" in the laboratory, which it is hoped would pave the way for new discoveries and for the possibility of screening drug candidates (see inset below). Our growing knowledge of the molecules involved in hearing mechanisms raises hopes for the future development of pharmacological treatments to repair some hearing impairments – a prospect that was unimaginable just a few years ago.

We are now working on the development of organoids composed of auditory sensory cells
Raphaël EtournayHead of the Cochlear Development and Therapeutic Prospects group at the Hearing Institute
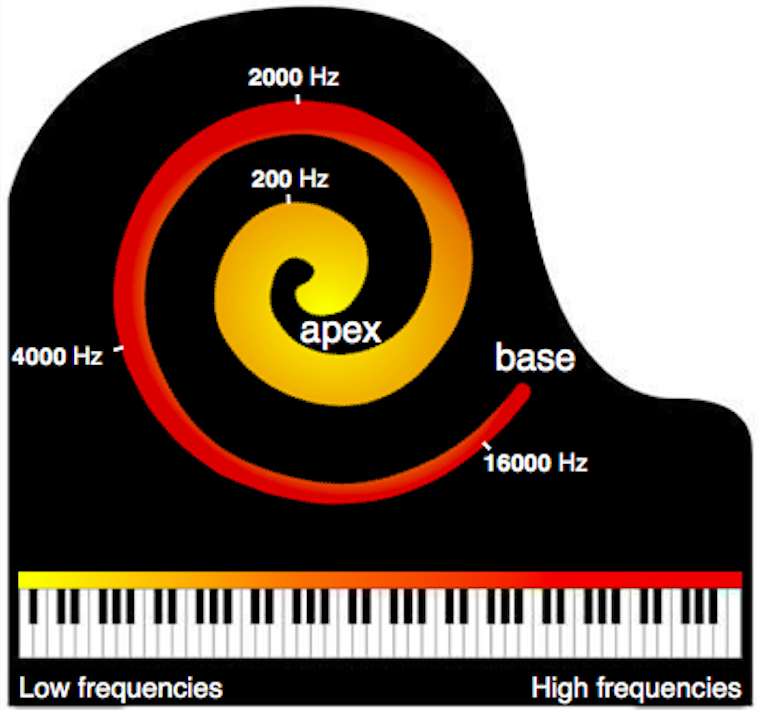
"Using stem cells, we are currently able to produce miniature organs measuring 1 to 2mm in diameter (organoids) composed of sensory cells from the balance organ, which is part of the inner ear. We are now working on the development of organoids composed of auditory sensory cells," explains Raphaël Etournay, Head of the Cochlear Development and Therapeutic Prospects group at the Hearing Institute. The cochlea, the auditory sensory organ, wound in a spiral shape, is lined with auditory sensory cells that can be thought of like a piano keyboard – each region deals with a specific frequency, with high sounds being picked up at the base of the spiral and low sounds at the other end. "Without necessarily reproducing a spiral, we are hoping to obtain this piano keyboard structure. We are studying the cellular and molecular mechanisms involved in the embryonic development of the cochlea, which gives us potential avenues to produce our organoids." Once they have been produced, these mini organs will be extremely useful for testing new therapies for hearing loss. "We could screen viral vectors for gene therapy or molecules capable of triggering the regeneration of auditory cells." The organoids could also be created from patient cells – cells that have been reprogrammed into stem cells (known as induced pluripotent stem cells or iPS cells) – for personalized medicine. Given the existence of such a wide variety of auditory impairments, that is a definite advantage.
Credit : AdobeStock
High hopes are also being placed on gene therapy, with a clinical trial for congenital hearing loss already planned in children and potential avenues for correcting hearing loss in adults in the future (see inset on gene therapy).
New therapeutic options are therefore under exploration. While early-onset hearing loss was the first to benefit from advances in research, scientists are now focusing on progressive hearing loss, especially late-onset hearing loss, presbycusis, which given the aging population represents a growing public health problem. Acoustic trauma (public enemy number one for hearing is excessive noise!), illness (20% of cases of hearing loss are caused by chronic ear infections), accidents (e.g. when diving) and drug toxicity are all factors that contribute to the destruction of the hair cells in the inner ear, which are not replenished in mammals (like us). Once thought to be irreversible, presbycusis could benefit from genetic, cellular or pharmacological preventive and curative treatments in future.
Research is also focusing on the "auditory" brain, about which little is known as yet. While most cases of hearing loss are related to the peripheral nervous system, some are also thought to result from impaired auditory perception in the brain. And there are still many unanswered questions.
What determines whether some sounds are perceived as pleasant or not? How do some medical conditions (such as autism and Alzheimer's) impair auditory perception and behaviors related to audio communication? How does the brain compensate for a hearing impairment? The recent opening of the first research center for hearing in France – the Hearing Institute, an Institut Pasteur center (see Interview) – will help boost this research and speed up the development of new diagnostic solutions and therapeutic approaches for hearing loss, which according to WHO will be the seventh leading cause of burden of disease by 2030.
Read the news: Presbycusis: ultra-rare genetic mutations responsible for a quarter of cases occurring around the age of 50.
 The Hearing Institute, an Institut Pasteur center, is expected to boost research and the creation of new diagnostic and therapeutic solutions for hearing loss. Copyright: Institut Pasteur.
The Hearing Institute, an Institut Pasteur center, is expected to boost research and the creation of new diagnostic and therapeutic solutions for hearing loss. Copyright: Institut Pasteur.

If the efficacy of this therapy is confirmed, it could be offered to infants at the age of around 3 to 5 months, as soon as the genetic diagnosis has been confirmed
Saaïd SafieddineJoint head of the Innovative Technologies and Hearing Loss Therapies group at the Hearing Institute
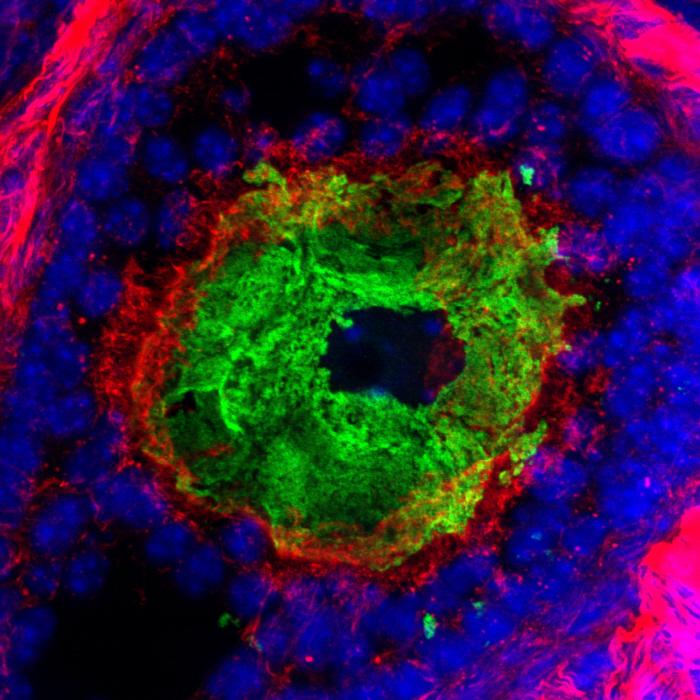
In 2019, Saaïd Safieddine's team in the unit led by Christine Petit at the Institut Pasteur (see Interview) published the results of a gene therapy technique that was found to durably reverse congenital hearing loss in experimental models. The technique involved an intracochlear injection of the OTOF gene (discovered by the Institut Pasteur team in 1999) in deaf adult mice, which are deficient in this gene. In humans, a deficiency in this gene leads to profound hearing loss owing to a lack of otoferlin, an essential protein for the transmission of sound information between the auditory sensory cells and the brain. By restoring intact protein production, the gene therapy was found to restore auditory thresholds to virtually normal levels in animal models. "We are currently preparing for a clinical trial with Necker-Enfants Malades Hospital in Paris," explains Saaïd Safieddine, currently joint head* of the Innovative Technologies and Hearing Loss Therapies group at the Hearing Institute. "If the efficacy of this therapy is confirmed, it could be offered to infants at the age of around 3 to 5 months, as soon as the genetic diagnosis has been confirmed," continues the scientist. In the cochlea there are two types of auditory sensory cell (inner and outer hair cells), surrounded by several types of support cell, which can all be targets depending on the gene involved. As well as raising hopes for infants born with a defective gene, it is thought that gene therapy could also be used to correct late-onset hearing loss. Christine Petit's laboratory, which for the past ten years has been working with Paul Avan to identify genes and genetic factors associated with presbycusis (late-onset sensorineural hearing loss) in humans, has recently shown that some forms of presbycusis could benefit from gene therapy – hence the development of these approaches in her laboratory and the convergence of this research with that led by Saaïd Safieddine.
"Among the genes that we are studying, some are also responsible for presbycusis – they speed up the aging of the inner ear," explains Saaïd, who is also working with the team led by Aziz El-Amraoui
*With Dr. Yann Nguyen, ENT specialist at Pitié-Salpêtrière Hospital in Paris.

A high-tech center for exploring hearing
The Center for Research and Innovation in Human Audiology (CERIAH) at the Hearing Institute will open in a few months on the Institut Pasteur campus in Paris, with a reception area for volunteers,* five audiometric booths, a large auditorium to test hearing in a variety of sound environments – with perfect phonic insulation, housed in the basement to avoid any extraneous noise –, and a virtual or augmented reality room to simulate situations that also involve balance, for example. "The aim of this platform is to develop and approve new protocols for exploring hearing," explains CERIAH director Professor Paul Avan, a biophysicist, physician and audiology expert. "Using psychoacoustic perception tests and electrophysiological measurements, our aim is to evaluate the hearing of individuals with or without hearing loss, with or without a hearing aid, in "real life" situations. It is possible to have a normal audiogram but to experience difficulties hearing in some sound environments. So we need to be able to fine-tune our assessment of hearing ability. Our protocols will be useful for diagnostics, monitoring therapies, measuring sound pollution and improving our understanding of auditory perception and cognition." Research will be carried out with other teams from the Hearing Institute and also with IRCAM (the French Institute for Research and Coordination in Acoustics/Music) and IRBA (the French Armed Forces Biomedical Research Institute), with a project on hearing damage caused by gunfire and constant noise.
* Volunteers will be recruited from the university student community and via hearing health professionals (ENT specialists, hearing aid specialists, etc.).

Paul Avan
Our protocols will be useful for diagnostics, monitoring therapies, measuring sound pollution and improving our understanding of auditory perception and cognition
How does hearing work?