What are the causes?
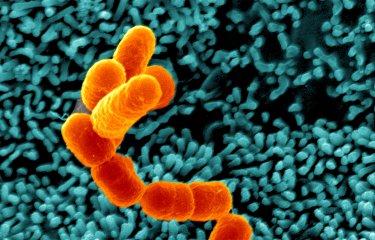
Shigellosis is caused by Shigella bacteria, which are specialized clones of Escherichia coli. Four Shigella serogroups have been identified (Shigella dysenteriae, Shigella flexneri, Shigella boydii and Shigella sonnei). The most common serogroup in France and other industrialized countries is S. sonnei. This serogroup is also emerging globally, including in low- and middle-income countries, where it is replacing S. flexneri.
How do the bacteria spread?
Shigellosis is a classic example of a disease related to poor hygiene. Shigella bacteria are spread by fecal-oral transmission. They are extremely infectious, with only 10 to 100 bacilli required to cause the disease. Humans are the sole reservoir and can eliminate these bacteria in their stools in the weeks following a dysenteric episode. In most cases, the disease is transmitted directly from patients to those around them. The disease can also be spread by flies and by fecally contaminated food or water containing Shigella bacteria. An increase in cases of shigellosis caused by sexual transmission (oral-anal sex) has also been observed in recent years in industrialized countries.
What are the symptoms?
The onset of the typical acute dysenteric form in adults occurs suddenly following a brief incubation period of 1 to 4 days after ingesting the bacteria. It is characterized by abdominal pain often combined with vomiting and frequent passage of purulent stools containing bloody mucus, which can in some cases be hemorrhagic. Patients experience high fever and a decline in their general condition.
Complications may occur over the course of the disease, particularly in infants and young children, causing severe forms of shigellosis that can potentially result in death.
The main acute complications are:
- hypoglycemia and gut-origin bacteremia or septicemia potentially complicated by septic shock
- dehydration due to fever and significant fluid and electrolyte loss through diarrhea, resulting in circulatory collapse and acute kidney failure
- hemolytic uremic syndrome and acute kidney failure of complex origin, which is fatal in most cases if patients cannot be treated quickly in an ICU, may be observed occasionally after contamination with the very rare strains of Shigella spp. that produce Shiga toxin
- toxic megacolon and intestinal obstruction potentially complicated by perforation with peritonitis.
The main chronic complications are a prolonged state of malnutrition with severe failure to thrive in young children.
How is shigellosis diagnosed?
Shigellosis diagnosis is confirmed by the detection of Shigella bacteria in a patient stool sample, whether by stool culture or molecular tests (polymerase chain reaction (PCR)) in a medical test laboratory. Conventional microbiological techniques are still the best way of confirming the serogroup and determining antibiotic sensitivity. All strains received at the CNR are now sequenced, enabling more precise typing that goes beyond the serogroup and also determines all the antibiotic-resistant genes in the bacterial strain.
What treatments are available?
Unlike other diarrheal diseases, shigellosis cannot be treated solely by rehydration. The bacteria invade the colonic mucosa, causing an inflammatory reaction that leads to destruction of infected tissue and even long-term complications. Antibiotic therapy generally results in rapid recovery without any sequelae. However, treatment has been complicated by the emergence of multidrug-resistant strains, particularly among S. sonnei and S. flexneri, which are often resistant to all traditional first-line antibiotics (ampicillin, tetracycline, sulfamethoxazole-trimethoprim, chloramphenicol, nalidixic acid), meaning that less accessible and much more expensive antibiotics are required (fluoroquinolones, third-generation cephalosporins and azithromycin). Strains that are resistant to all these antibiotics are starting to be detected in several countries. In France, these highly drug-resistant strains, first detected in 2015, are now responsible for approximately 10% of shigellosis cases each year.(1)
How can shigellosis be prevented?
As with all diarrheal diseases, preventive measures focus on improving hygiene: better education on personal hygiene, latrine construction, fly control, regulations on the use of human fecal matter in agriculture, and a clean drinking water supply. Unfortunately, such improvements do not appear a realistic prospect in many regions of the world that have seen rapid population expansion, particularly in urban areas. Vaccine development is therefore an important and urgent priority. Preventive work on this new sexually transmitted infection is necessary in the male homosexual community.
Who is affected?
Given the conditions in which it occurs, the disease mainly affects children living in poor and overpopulated regions of the world where health infrastructure and personal hygiene are inadequate. It can also affect soldiers on operations in these regions, humanitarian workers and tourists. In industrialized nations, small-scale outbreaks of S. sonnei may occur among groups of young children or in religious communities. In recent years, S. sonnei and S. flexneri have become epidemic in the male homosexual community.
How many people are affected?
Shigellosis causes approximately 200,000 deaths per year globally, including 65,000 deaths in children under the age of five. In France, the frequency of this pathogen has increased considerably in recent years, with 1,595 strains received by the CNR in 2023 (compared with 700-1,100 strains annually between 2005 and 2017).(1)
November 2024