In May 2020, while the first wave of the COVID-19 outbreak was coming to an end in France, initial reports emerged of patients with some persistent symptoms several weeks or months post-infection. This phenomenon, now referred to as "long COVID" (or post-COVID-19 syndrome) affects over 20% of patients after 5 weeks and over 10% of patients after 3 months. Serious or severe forms of initial SARS-CoV-2 infection appear to be risk factors in the onset of long COVID.
The most common prolonged symptoms affecting patients post-COVID-19 are fatigue (which may be severe in some cases), neurological disorders (loss of taste and smell, headaches, and even cognitive decline), heart and respiratory disorders, digestive problems, psychiatric disorders and skin conditions. Current treatments are largely symptomatic with an emphasis on rehabilitation and remedial therapy, often combined with psychological support. Research is being conducted on repurposing drugs used to treat similar symptoms for other diseases.
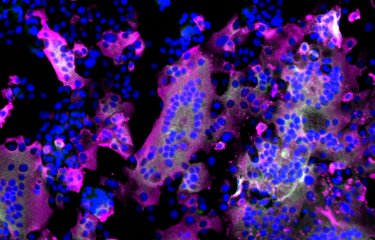
Although the data is still limited, it appears that the prognosis for patients with long COVID is positive. Research on long COVID mechanisms has revealed that the condition may be caused by damage from initial infection as well as viral persistence and inflammation in some areas of the human body. One study* on anosmia showed that the SARS-CoV-2 virus is detectable in the olfactory epithelium for several months. The olfactory epithelium may provide a gateway to the brain and explain some neurological signs of long COVID.
Illustration of a healthy mucosa and a mucosa infected with the SARS-CoV-2 virus with persistence

* This study was conducted by Pierre-Marie Lledo, Head of the Perception and Memory Unit (Institut Pasteur/CNRS), Hervé Bourhy, Head of the Lyssavirus, Epidemiology and Neuropathology Unit at the Institut Pasteur (Université de Paris) and Marc Lecuit, Head of the Biology of Infection Unit (Institut Pasteur, Inserm, Université de Paris, AP-HP).