What are the causes?
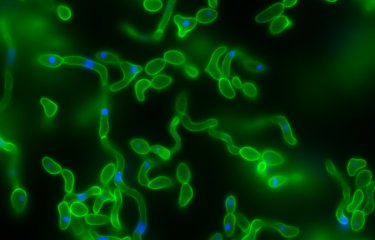
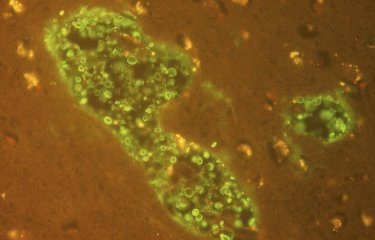
The main infectious agent responsible for cryptococcosis is the fungus Cryptococcus neoformans, an encapsulated yeast mainly spread by airborne transmission that is present in soil and organic debris. The geographical distribution of Cryptococcus neoformans is widespread; the pathogen is found all over the world. Cryptococcus gattii is less widespread and is mainly found in certain tree species in tropical areas.
How does the disease spread?
The fungus Cryptococcus neoformans is present in the environment, and contamination generally occurs by inhalation. Direct inoculation via skin wounds can cause skin lesions such as paronychia or cellulitis, and the infection can sometimes spread to other parts of the body in immunocompromised patients. But there is no human-to-human transmission, apart from some rare observations reported after organ transplants. Rare cases have been reported in people who have cleaned surfaces that were highly contaminated with pigeon droppings, and close contact with pigeons is therefore not recommended for immunocompromised individuals. Cryptococcus gattii is found in trees such as eucalyptus and is also spread by inhalation.
What are the symptoms?
The most common clinical form of cryptococcosis is disseminated meningoencephalitis (in more than 60% of cases, and in more than 90% of cases in patients with HIV). The symptoms are variable: headache and moderate fever are experienced by more than 70% of patients, while dizziness, irritability, confusion, convulsions, drowsiness or even coma, cranial nerve palsy and motor deficiency may occur in 20 to 50% of cases. Rapid development of symptoms and signs of intracranial hypertension can indicate a poor prognosis. In the absence of treatment, worsening of symptoms and death are inevitable. With treatment, premature mortality still occurs in around 28% of non-HIV patients and 15% of patients with HIV.
Infection can also be localized to the lungs, leading to a pneumonia-like illness with non-specific symptoms (cough and moderate fever), or to any other organ. Skin lesions caused when the yeast spreads in the bloodstream can appear as painless papules that can become ulcerous. Some patients are asymptomatic. Infection is diagnosed by direct examination or histology to determine the presence of yeast surrounded by a clear halo in tissue or fluid samples; by the identification of Cryptococcus neoformans in these samples; and/or by the detection of the specific antigen in a blood serum or cerebrospinal fluid sample. Rapid tests have been developed for bedside diagnosis.
How can cryptococcosis be prevented?
Prevention of cryptococcosis in people at risk, especially immunocompromised individuals, may include measures to avoid exposure to dusty environments or areas with bird droppings.
There is currently no preventive vaccine for the disease.
What treatments are available?
Several weeks of antifungal treatment is required. In severe cases (meningoencephalitis and severe pulmonary disease), treatment involves a combination of liposomal amphotericin B and 5-fluorocytosine, followed by high-dose fluconazole. In the event of intracranial hypertension, lumbar punctures are also performed. Clinical improvement is generally slow, taking one to two weeks, and remission is only achieved after at least six weeks of initial treatment. Sequelae may remain after recovery. Prophylactic treatment for relapses is systematically administered in HIV patients until full, stable immune reconstitution has been achieved with antiretroviral therapy.
There is currently no curative vaccine for the disease.
Who is affected?
Although anyone can be infected with Cryptococcus spores, immunocompromised individuals are particularly vulnerable to severe infections, such as those living with HIV/AIDS (cryptococcosis is a typically opportunistic infection in immunocompromised HIV patients with a CD4 count of less than 200/mm3), organ transplant recipients, or people with a systemic disease or blood disorder.
How many people are affected?
Cryptococcosis is responsible for 19% of deaths associated with human immunodeficiency virus (HIV) in HIV-positive patients who have received little or no treatment, most of which occur in subtropical or tropical regions (especially Sub-Saharan Africa).
In France, around 40% of cryptococcosis cases are HIV-related.
November 2024