Sex determination is the process whereby an organism becomes male or female. A multinational consortium, led by Institut Pasteur scientists, has made a breakthrough in understanding the genetics of sex determination in humans. They have discovered that DHX37, a gene highly conserved during evolution and until now only known for its role in ribosome biogenesis, is involved in both determining and maintaining the identity of testicular tissue. It is the first genetic cause to be identified for testicular regression. These findings open up new avenues for understanding the genetic origin of disorders of sex development (DSD). It will be published in the journal Genetics in Medicine and is available online.
DSDs are defined as congenital conditions with discordant development of chromosomal and gonadal/anatomical sex and cover a wide range of phenotypes that involve the endocrine and reproductive systems. Most of these conditions lead to sexual ambiguity at birth but some can only be diagnosed in adulthood. Testicular regression syndrome is a rare disease characterized by the uni- or bilateral absence of testes and has an embryonic origin. This syndrome affects roughly one in 2,000 boys. It represents approximately 32,700 births per year in the world and, in France represents about 180 births annually.
Using genomic approaches and in partnership with various universities and foreign hospitals, scientists from the Institut Pasteur have identified recurrent de novo mutations in individuals with DSD. These mutations are localized in highly conserved domains of gene DHX37, which codes for the protein DHX37.
Their findings show that 11% of patients with complete failure of testicular determination carry mutations in this gene. In addition, 25% of boys with testicular regression syndrome, which is also known as vanishing testis syndrome, carry pathogenic mutations in this gene. These figures point to mutations in DHX37 as a major cause of DSD.
"It is the first time that a genetic cause has been identified for testicular regression. The gene we have identified plays an essential role in testicular determination, and it is necessary to have a healthy gene for both testicle development and maintenance of testicular tissue. Our findings also prove that mutations in gene DHX37 are one of the most common causes of sex-reversal identified in humans." Dr Ken McElreavey, lead author of the paper and Head of the Human Developmental Genetics Unit at the Institut Pasteur.
DHX37 is a protein that has been highly conserved during evolution. It is known for being essential for biogenesis of the ribosome, and more specifically of its small subunit. "The relationship between protein DHX37 and the "pro-male" and "pro-female" regulation pathways involved in sex determination is completely unknown and it is a totlally unexpected discovery", explains Dr McElreavey.
This new data indicates that some DSDs should be added to the list of ribosomopathies. Ribosomopathies are human diseases associated with ribosome biogenesis or function. They are part of an emerging and, for the moment, poorly understood field of medicine. It is still unclear to the scientific community how the variants of proteins involved in ribosome biogenesis or function produce different and highly specific human phenotypes.
Dr Anu Bashamboo, the senior author of the paper and Institut Pasteur scientist explains: "Given its dual role in ribosome biogenesis and sex determination, protein DHX37 has forced us to reconsider sex-detemination in humans. Our results are a paradigm shift in understanding DSDs and the broader mechanisms involved in sex determination in vertebrates. It also opens up new avenues for research to shed light on the relationship between ribosomes and human diseases."
- More information -
Sex determination
Sex determination is the process whereby an organism becomes male or female. However, the components and mechanisms involved in sex determination in vertebrates remain largely unknown. Recent data, from the Institut Pasteur Human Developmental Genetics Unit, show that the choice of forming a testicle or ovary in mammals is the result of a molecular conflict between antagonistic "pro-male" and "pro-female" regulatory networks. A powerful and unbiased approach for understanding these mechanisms involves carrying out genomic screening on patients with DSD, to identify the mutations responsible for the disease.
Testicular regression syndrome (ORPHA 983)
XY gonadal dysgenesis, also known as "testicular regression syndrome", is a rare disease. It includes a wide range of internal and external genital anomalies, linked to a testicular development disorder arising between the 8th and 14th week of fetal growth. The phenotype varies according to when the in utero gonadal regression occurs. It ranges from a female phenotype to a male phenotype with anorchia (absence of testes) in patients with a 46,XY karyotype. If testicular regression occurs early, between 8 and 10 weeks of pregnancy, the phenotype is female with or without ambiguity of external genitalia, an absence of gonads and a hypoplastic uterus. If regression occurs after 12 weeks, the phenotype is male presenting with anorchia or hypoplastic testicles.
Ribosomes and ribosomopathies
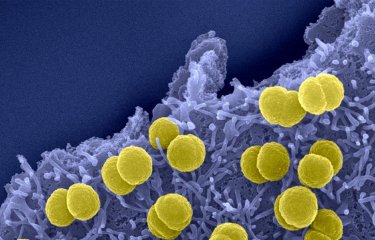
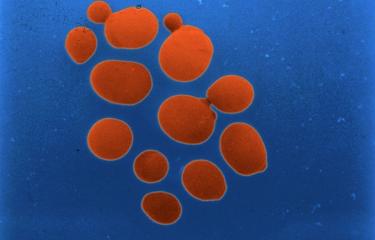
Ribosomes are complexes of messenger RNA (mRNA) and proteins that have been highly conserved during evolution. Their role is to synthesize proteins by decoding information contained in the mRNA. Ribosomes are made up of two subunits, a smaller one that "reads" the mRNA and a larger one that handles polymerization of amino acids to form the corresponding protein.
Ribosome diseases, or ribosomopathies, are diseases associated with a ribosome disorder. These disorders can affect ribosome structure or function (at both messenger RNA or ribosome protein level), or a gene linked to ribosome biogenesis. Most ribosomopathies are classified as rare genetic diseases. They include Diamond–Blackfan anemia (DBA), a congenital erythroid aplasia, where the bone marrow is unable to produce a sufficient amount of red blood cells and Treacher Collins syndrome, a mandibulofacial dysostosis characterized by facial deformities.
Source
Pathogenic variants in the DEAH-box RNA helicase DHX37 are a frequent cause of 46,XY gonadal dysgenesis and 46,XY testicular regression syndrome. Genetics in Medicine. July 24, 2019.
McElreavey K, Jorgensen A, Eozenou C, Merel T, Bignon-Topalovic J, Tan DS, Houzelstein D, Buonocore F, Warr N, Kay RGG, Peycelon M, Siffroi JP, Mazen I, Achermann JC, Shcherbak Y, Leger J, Sallai A, Carel JC, Martinerie L, Le Ru R, Conway GS, Mignot B, Van Maldergem L, Bertalan R, Globa E, Brauner R, Jauch R, Nef S, Greenfield A, Bashamboo A.
DOI : 10.1038/s41436-019-0606-y